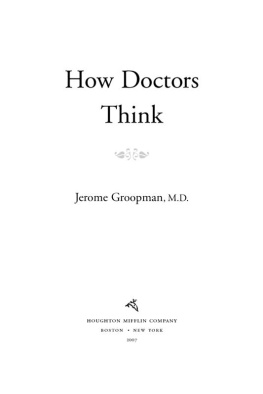
Groopman - How Doctors Think
Here you can read online Groopman - How Doctors Think full text of the book (entire story) in english for free. Download pdf and epub, get meaning, cover and reviews about this ebook. year: 2008, publisher: Houghton Mifflin Harcourt, genre: Art. Description of the work, (preface) as well as reviews are available. Best literature library LitArk.com created for fans of good reading and offers a wide selection of genres:
Romance novel
Science fiction
Adventure
Detective
Science
History
Home and family
Prose
Art
Politics
Computer
Non-fiction
Religion
Business
Children
Humor
Choose a favorite category and find really read worthwhile books. Enjoy immersion in the world of imagination, feel the emotions of the characters or learn something new for yourself, make an fascinating discovery.
How Doctors Think: summary, description and annotation
We offer to read an annotation, description, summary or preface (depends on what the author of the book "How Doctors Think" wrote himself). If you haven't found the necessary information about the book — write in the comments, we will try to find it.
How Doctors Think — read online for free the complete book (whole text) full work
Below is the text of the book, divided by pages. System saving the place of the last page read, allows you to conveniently read the book "How Doctors Think" online for free, without having to search again every time where you left off. Put a bookmark, and you can go to the page where you finished reading at any time.
Font size:
Interval:
Bookmark:
Copyright 2007 by Jerome Groopman
All rights reserved
For information about permission to reproduce selections from this book, write to Permissions, Houghton Mifflin Company, 215 Park Avenue South, New York, New York 10003.
Visit our Web site: www.hmhco.com.
The Library of Congress has cataloged the print edition as follows:
Groopman, Jerome E.
How doctors think / Jerome Groopman.
p. cm.
Includes bibliographical references and index.
ISBN -13: 978-0-618-61003-7
ISBN -10: 0-618-61003-0
1. MedicineDecision making. 2. Medical logic.
3. PhysiciansPsychology. 1. Title.
R723.5.G75 2007
610dc22 2006035718
e ISBN 978-0-547-34863-6
v2.0115
The illustration on page 139 is by Michael Prendergast
AUTHORS NOTE
In order to protect their privacy, the names and certain identifying characteristics of all of the patients whose medical histories are
described in this book have been changed. In addition, Dr. Karen Delgado, Dr. Bert Foyer, Dr. Wheeler, Rick Duggan, and Drs. A, B, C, D, and E are fictitious names.
FOR MY MOTHER
Ayshet chayil
( a woman of valor)
We carve out order by leaving the
disorderly parts out.
William James
A NNE DODGE HAD LOST COUNT of all the doctors she had seen over the past fifteen years. She guessed it was close to thirty. Now, two days after Christmas 2004, on a surprisingly mild morning, she was driving again into Boston to see yet another physician. Her primary care doctor had opposed the trip, arguing that Annes problems were so long-standing and so well defined that this consultation would be useless. But her boyfriend had stubbornly insisted. Anne told herself the visit would mollify her boyfriend and she would be back home by midday.
Anne is in her thirties, with sandy brown hair and soft blue eyes. She grew up in a small town in Massachusetts, one of four sisters. No one had had an illness like hers. Around age twenty, she found that food did not agree with her. After a meal, she would feel as if a hand were gripping her stomach and twisting it. The nausea and pain were so intense that occasionally she vomited. Her family doctor examined her and found nothing wrong. He gave her antacids. But the symptoms continued. Anne lost her appetite and had to force herself to eat; then shed feel sick and quietly retreat to the bathroom to regurgitate. Her general practitioner suspected what was wrong, but to be sure he referred her to a psychiatrist, and the diagnosis was made: anorexia nervosa with bulimia, a disorder marked by vomiting and an aversion to food. If the condition was not corrected, she could starve to death.
Over the years, Anne had seen many internists for her primary care before settling on her current one, a woman whose practice was devoted to patients with eating disorders. Anne was also evaluated by numerous specialists: endocrinologists, orthopedists, hematologists, infectious disease doctors, and, of course, psychologists and psychiatrists. She had been treated with four different antidepressants and had undergone weekly talk therapy. Nutritionists closely monitored her daily caloric intake.
But Annes health continued to deteriorate, and the past twelve months had been the most miserable of her life. Her red blood cell count and platelets had dropped to perilous levels. A bone marrow biopsy showed very few developing cells. The two hematologists Anne had consulted attributed the low blood counts to her nutritional deficiency. Anne also had severe osteoporosis. One endocrinologist said her bones were like those of a woman in her eighties, from a lack of vitamin D and calcium. An orthopedist diagnosed a hairline fracture of the metatarsal bone of her foot. There were also signs that her immune system was failing; she suffered a series of infections, including meningitis. She was hospitalized four times in 2004 in a mental health facility so she could try to gain weight under supervision.
To restore her system, her internist had told Anne to consume three thousand calories a day, mostly in easily digested carbohydrates like cereals and pasta. But the more Anne ate, the worse she felt. Not only was she seized by intense nausea and the urge to vomit, but recently she had severe intestinal cramps and diarrhea. Her doctor said she had developed irritable bowel syndrome, a disorder associated with psychological stress. By December, Annes weight dropped to eighty-two pounds. Although she said she was forcing down close to three thousand calories, her internist and her psychiatrist took the steady loss of weight as a sure sign that Anne was not telling the truth.
That day Anne was seeing Dr. Myron Falchuk, a gastroenterologist. Falchuk had already gotten her medical records, and her internist had told him that Annes irritable bowel syndrome was yet another manifestation of her deteriorating mental health. Falchuk heard in the doctors recitation of the case the implicit message that his role was to examine Annes abdomen, which had been poked and prodded many times by many physicians, and to reassure her that irritable bowel syndrome, while uncomfortable and annoying, should be treated as the internist had recommended, with an appropriate diet and tranquilizers.
But that is exactly what Falchuk did not do. Instead, he began to question, and listen, and observe, and then to think differently about Annes case. And by doing so, he saved her life, because for fifteen years a key aspect of her illness had been missed.
This book is about what goes on in a doctors mind as he or she treats a patient. The idea for it came to me unexpectedly, on a September morning three years ago while I was on rounds with a group of interns, residents, and medical students. I was the attending physician on general medicine, meaning that it was my responsibility to guide this team of trainees in its care of patients with a wide variety of clinical problems, not just those in my own specialties of blood diseases, cancer, and AIDS. There were patients on our ward with pneumonia, diabetes, and other common ailments, but there were also some with symptoms that did not readily suggest a diagnosis, or with maladies for which there was a range of possible treatments, where no one therapy was clearly superior to the others.
I like to conduct rounds in a traditional way. One member of the team first presents the salient aspects of the case and then we move as a group to the bedside, where we talk to the patient and examine him. The team then returns to the conference room to discuss the problem. I follow a Socratic method in the discussion, encouraging the students and residents to challenge each other, and challenge me, with their ideas. But at the end of rounds on that September morning I found myself feeling disturbed. I was concerned about the lack of give-and-take among the trainees, but even more I was disappointed with myself as their teacher. I concluded that these very bright and very affable medical students, interns, and residents all too often failed to question cogently or listen carefully or observe keenly. They were not thinking deeply about their patients problems. Something was profoundly wrong with the way they were learning to solve clinical puzzles and care for people.
You hear this kind of criticismthat each new generation of young doctors is not as insightful or competent as its forebearsregularly among older physicians, often couched like this: When I was in training thirty years ago, there was real rigor and we had to know our stuff. Nowadays, well... These wistful, aging doctors speak as if some magic that had transformed them into consummate clinicians has disappeared. I suspect each older generation carries with it the notion that its time and place, seen through the distorting lens of nostalgia, were superior to those of today. Until recently, I confess, I shared that nostalgic sensibility. But on reflection I saw that there also were major flaws in my own medical training. What distinguished my learning from the learning of my young trainees was the nature of the deficiency, the type of flaw.
Next pageFont size:
Interval:
Bookmark:
Similar books «How Doctors Think»
Look at similar books to How Doctors Think. We have selected literature similar in name and meaning in the hope of providing readers with more options to find new, interesting, not yet read works.
Discussion, reviews of the book How Doctors Think and just readers' own opinions. Leave your comments, write what you think about the work, its meaning or the main characters. Specify what exactly you liked and what you didn't like, and why you think so.