Contents
Copyright 2017 by Patsy Catsos
Foreword copyright 2017 by William D. Chey
Photographs copyright 2017 by Andrew Purcell
All rights reserved.
Published in the United States by Harmony Books, an imprint of the Crown Publishing Group, a division of Penguin Random House LLC, New York.
www.crownpublishing.com
Harmony Books is a registered trademark, and the Circle colophon is a trademark of Penguin Random House LLC.
Two previous editions were self-published in paperback as IBSFree at Last! by Pond Cove Press, Portland, Maine, in 2009 and 2012. Copyright 2008, 2012, by Patsy Catsos, MS, RD, LD.
Library of Congress Cataloging-in-Publication Data is available.
ISBN9780451497727
Ebook ISBN9780451497734
Illustrations on by Ellen Byrne
Illustration on by Designua/Shutterstock
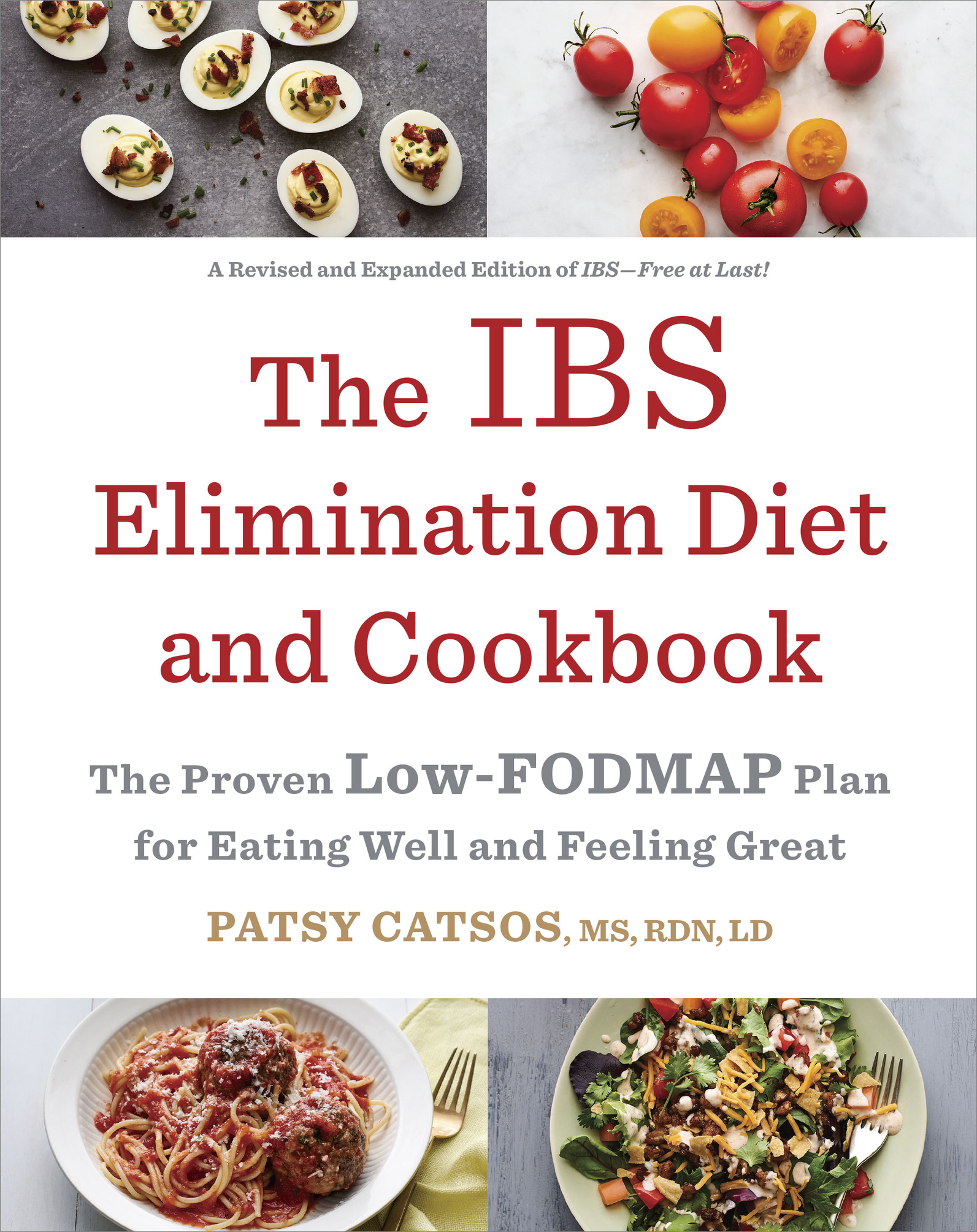
Cover design by Jennifer Carrow
Cover photographs by Andrew Purcell
v4.1
a
This book is dedicated to my parents,
for their patient instruction in cooking and in life,
their steadfast love and encouragement,
and with appreciation for their generous and creative hearts.
Contents
Foreword
I rritable Bowel Syndrome or IBSthe name conjures up different images and connotations for different people. For the unaffected public, popular movies like Along Comes Polly and Ladykillers put IBS in a comical light. Who can forget a panicked Reuben Feffer, played by Ben Stiller, watching helplessly after an ill-advised ethnic dinner leads to an overflowing toilet? For IBS sufferers, this condition is anything but comical. Imagine if you were a patient with belly pain and bowel problems in search of solutions, and your doctor told you the following: IBS is a disorder without a known cause, except, of course, that IBS might be caused by depression and/or anxiety (its all in your head), that it is chronic and will last a lifetime (learn to live with it), that there are lots of other diseases that can masquerade as IBS so it is diagnosed only after doing lots of tests, and medical treatments can sometimes work but can cause potentially dangerous side effects. One can see why words like embarrassment, frustration, hopelessness, and isolation are so commonly used by patients to describe their IBS.
For health-care providers, IBS is a scary, frustrating disorder as wellno clear cause, a chronic clinical course requiring repeated visits and phone calls, lots of doubts about assigning the diagnosis, and no cureworse yet, the available medical treatments provide only modest benefits when compared to a placebo pill. Another group that has only recently entered the discussion is third-party payersthe government and private insurance companies that provide payment for medical services. Ask any doctor, and they will tell you that the most important determinant of services they render and the medications they prescribe are what a patients insurance company will pay for. Increasingly, payers are refusing to pay for drugs to treat IBS or put up so many roadblocks that patients and doctors get frustrated and give up trying to provide the newer prescription drugs. In their defense, payers have to make difficult choices when considering what medications to pay for. With every breakthrough drug for life-threatening diseases like hepatitis C, HIV, and cancer, there is less money for quality of life disorders like IBS. After all, IBS doesnt kill anyone and is really just an inconvenience, not a real diseaseright? So, add limited access to newer, more expensive prescription drugs to the long list of problems facing IBS patients.
So, is it a surprise that IBS patients are veering from the traditional treatment model that relies so heavily on over-the-counter and prescription medications? More and more, patients are looking for holistic solutions for their IBS symptoms. As is often the case, answers may be hiding in plain sight. Consider for a moment that at least two-thirds of IBS sufferers associate symptom onset or worsening with eating a meal. Despite this association being known for many years, it has only been over the last decade that food has re-emerged as a potentially important cause and solution for patients with IBS. When I was training to become a gastroenterologist at the University of Michigan in the early 1990s, I was taught that there was no clear association between eating a meal and the development of symptoms and that there were no effective diet interventions for IBS. At that time, like nearly all other major medical centers in the United States, we did not have a dietitian who worked within the GI division. On the rare occasion that we referred a patient to our hospital dietitians, the consultation was typically to address enteral nutrition or total parenteral nutrition. We rarely, if ever, referred IBS patients for outpatient nutrition counseling. Fast forward to the current day, and how things have changed. At the University of Michigan, we now have full-time dietitians embedded within the Division of Gastroenterology. Our dietitians are experts in GI nutrition and, rather than viewed as subordinates, are considered to be valued members of our multidisciplinary health-care team. Our experience and the experiences of others who have created similar care models for patients with complex GI issues have validated that the team is greater than the sum of its parts.
We have entered a new age, one in which there is a growing recognition of the importance of diet and lifestyle in the care of patients with complex GI issues like IBS. We are finally at a time in which there are evidence-based dietary treatments for IBS patients. At present, the greatest weight of evidence supports a role for dietary restriction of fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs) as a treatment for IBS. Our group, as well as others, has conducted clinical trials that demonstrate benefits of the low-FODMAP diet for IBS symptoms, particularly pain and bloating, as well as quality of life. Now that the efficacy discussion has started to wind down, attention has turned to the best ways in which to administer the diet in a medically responsible fashion. Though the diet can be quite effective for some, it isnt a panacea for all. Also, the low-FODMAP diet is fairly complex with elimination and reintroduction phases. To maximize the likelihood of benefit, the elimination and reintroduction phases of the diet must be administered properly. The low-FODMAP diet is optimally administered with the assistance of a properly trained health provider, ideally a registered dietitian. However, sometimes a dietitian wont be available, or a person will just want to learn about the low-FODMAP diet from a credible source. That is where The IBS Elimination Diet and Cookbook can be an invaluable resource.
It must be acknowledged that Patsy Catsos was a trailblazer when she published IBSFree at Last! in 2009. When I first read this book, it provided a new construct within which to consider IBS. It can be said that IBSFree at Last! was ahead of its time and helped to usher in the low-FODMAP era in the United States. Given the rapid expansion in knowledge around all aspects of IBS in general and the low-FODMAP diet specifically, the timing is right for an updated how-to manual like The IBS Elimination Diet and Cookbook. Readers will gain an understanding of IBS; why the low-FODMAP diet works for many IBS patients; a guide to eliminating FODMAPs from your diet; if you improve, how to reintroduce foods containing FODMAPs to allow you to broaden your diet as much as tolerated; and lots of helpful tips and recipes. For patients with IBS,