Copyright 2015 Michelle Stewart
15 16 17 18 19 5 4 3 2 1
All rights reserved. No part of this book may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, without the prior written consent of the publisher or a license from The Canadian Copyright Licensing Agency (Access Copyright). For a copyright license, visit www.accesscopyright.ca or call toll free to 1-800-893-5777.
Published by LifeTree Media Ltd.
www.lifetreemedia.com
Distributed by Greystone Books Ltd.
www.greystonebooks.com
Cataloguing data available from Library and Archives Canada
ISBN 978-1-928055-13-6 (paperback)
ISBN 978-1-928055-14-3 (epub)
ISBN 978-1-928055-15-0 ( PDF )
Editing by Maggie Langrick
Copyediting by Carol Volkart
Cover design by David Drummond
Foreword
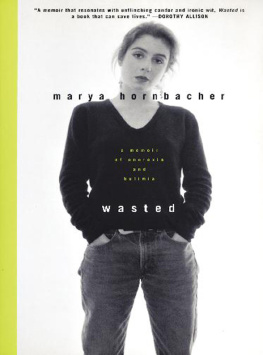
This compelling story of the last year in the life of an individual dying from her chronic anorexia and bulimia is at once spellbinding and terribly sad. While the author does not deliberately dwell on her eating disorder, to me it shouts out from every page as the most consistent aspect of the final part of her life. Michelle Stewarts heartbreaking acknowledgment in an entry when it is clear her renal failure has progressed to the point that she has little time remaining that she continues to weigh herself four times per day and restrict her eating to attempt to avoid gaining weight is a telling commentary on the vicious grip that anorexia exerts on its victims.
Of course this grip is evident in so many ways in Michelles life. Her decision to not have life-saving dialysis because it would require some changes in her eating is her anorexia in direct action. The disruption of so many relationships, and so many aspects of her life over decades is a direct consequence of her condition. As she attempts to have the best life she can have, her dual eating disorder is her constant companion her worst best friend ever.
Anorexia nervosa, along with its related diagnoses of bulimia and other forms of eating disorder, is a serious medical illness with significant mortality and endless suffering. The death rate from eating disorders is between 10 and 20 per cent, making it one of the most lethal psychiatric conditions. The rate of development of chronic, intractable illness is an additional 10 to 15 per cent. These latter individuals struggle to uphold their quality of life in the face of seemingly insurmountable obstacles.
The illness has been reported in medical literature since the late 1600s, and occurs all over the world in both men and women. It is recognized wherever there is a segment of society that has adequate access to food, and where starvation is rare. Although the manifestations of this illness are somewhat affected by local cultures, its form is overwhelmingly so similar across regional boundaries that it remains one of the most identifiable psychiatric conditions. When examined genetically, the proportion of risk for eating disorders attributable to underlying genetic vulnerability is 75 to 80 per cent, the highest of any psychiatric illness.
Despite these facts, individuals with anorexia and bulimia face discrimination at multiple levels. The first of those arises when family, society and even the health-care system questions whether the condition is actually an illness at all, mistakenly asserting that it is a voluntary choice on the part of the sufferer. This is a soul-destroying situation for the affected individual, causing her to invalidate her own suffering, and making her reluctant to seek out help.
The author describes clearly the sequence of a sexual assault leading to the development of her fatal eating disorder, and makes it clear throughout the book that the condition is not really about the food. Rather, food is a symptom of all the other things that were wrong when she fell ill, and which have gone wrong since, none of which ever received adequate attention from her health-care providers, over so many years of treatment.
When a sufferer of eating disorders does come to seek treatment, a second layer of discrimination comes into play. Access to effective treatment is non-existent throughout many parts of Canada, and where treatment exists, there are long waiting periods, even for those most severely affected. Well-meaning but poorly trained individuals who end up attempting to look after these individuals often make damaging suggestions, such as the one made to Michelle Stewart although she was a survivor of sexual assault that getting a boyfriend and having sex might help her recover from her illness. Other practitioners will hold on to outdated theories about the cause of anorexia and lay the blame on the victims family, alienating the patient from his or her most important source of support and assistance through recovery.
And why are practitioners so poorly prepared? In Toronto, which hosts the largest program for anorexia in Canada, medical students receive no education about eating disorders. Family Medicine residents receive no formal education in eating disorders. The psychiatric training program, one of the largest in North America, devotes a total of three hours out of a five-year program to eating disorders education. Most residents graduating from this program have never seen an individual with anorexia.
Finally, there is the systemic discrimination against those with this type of psychiatric disorder, which is especially prevalent in young female sufferers of mental illnesses. If anorexia were an illness primarily affecting middle-aged men as is prostate cancer, for example I believe there would be a clinic in every hospital in the country, and riots in the street if there were delays in treatment. The mortality from anorexia is in the same range as that for prostate cancer.
A final source of discrimination, which is particularly shattering for many patients, is the notion that recovery from anorexia is not possible, and that the best a sufferer can hope for is to learn to live with her illness. Although it is totally untrue, this view is endorsed by well-meaning but poorly informed health-care practitioners who, lacking training and experience, do not see good results in their own practice, and thus assume that a good result is not achievable. This robs the affected person of any hope for the future, and all too many of those who suffer make the choice made by Michelle to make the best of it, and simply struggle to do the best they can for as long as possible.
Recovery from anorexia is definitely possible in fact, it is the most common outcome overall. While earlier detection and treatment is associated with a greater likelihood of recovery, I have seen patients who have been ill for more than 40 years make complete recoveries. Most recoveries occur sometime in the first 15 years duration of illness, and the average time to recover is six to seven years after the onset of the condition. The overall rate of recovery is 60 to 70 per cent. So I rarely advise families or patients to accept their condition as untreatable, especially if they are young.
What does recovery look like? After one year, the patient will talk about the challenges of maintaining a recovered state, and although she or he has some confidence that it can be maintained, there may still be a feeling of hesitancy. She may have occasional bad days, and some ongoing concerns about her body, but she is aware that her life is moving forward in a positive way.
After two years, most recovered individuals will tell me that they feel very solid in their recovery and comfortable in their body, and that they really no longer think about food, weight or shape. They tell me a lot about their new life.
After five years, most recovered individuals tell me that they can barely remember having been ill; that it seems like a dream, like it happened to someone else. They tend to tell me a lot about how their life has been going since they got better. This is the state that individuals suffering from this terrible illness can and should hope for.
Next page