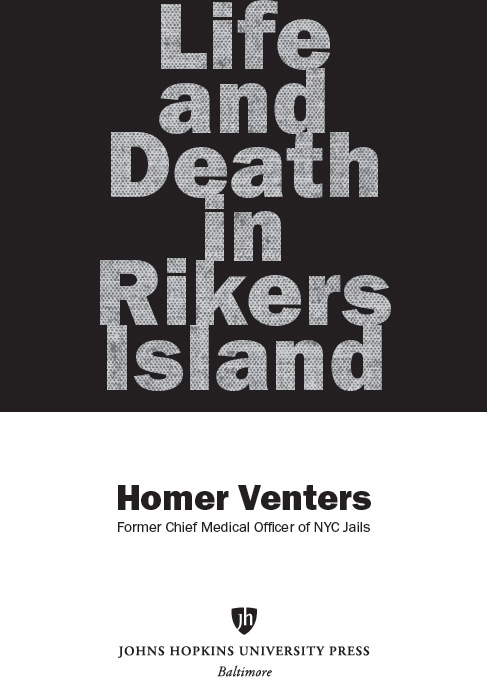
Life and Death in Rikers Island
To Susan. You know what you did.
2019 Johns Hopkins University Press
All rights reserved. Published 2019
Printed in the United States of America on acid-free paper
9 8 7 6 5 4 3 2 1
Johns Hopkins University Press
2715 North Charles Street
Baltimore, Maryland 21218-4363
www.press.jhu.edu
Library of Congress Cataloging-in-Publication Data
Names: Venters, Homer, 1967 author.
Title: Life and death in Rikers Island / Homer Venters.
Description: Baltimore : Johns Hopkins University Press, 2019. | Includes bibliographical references and index.
Identifiers: LCCN 2018023724 | ISBN 9781421427355 (pbk. : alk. paper) | ISBN 9781421427362 (electronic) | ISBN 1421427354 (pbk. : alk. paper) | ISBN 1421427362 (electronic)
Subjects: | MESH: New York (N.Y.). Department of Correction. | Prisons | Delivery of Health Care | Prisoners | Health Status | Health Risk Behaviors | Human Rights Abuses | New York City
Classification: LCC RA448.N5 | NLM WA 300 AN7 | DDC 362.109747/1dc23
LC record available at https://lccn.loc.gov/2018023724
A catalog record for this book is available from the British Library.
Special discounts are available for bulk purchases of this book. For more information, please contact Special Sales at 410-516-6936 or .
Johns Hopkins University Press uses environmentally friendly book materials, including recycled text paper that is composed of at least 30 percent post-consumer waste, whenever possible.
Acknowledgments
THERE ARE MANY PEOPLE who have opened my eyes to the health risks of jail. Ive benefited from working with a team of mission-driven people who have improved the lives of many thousands of patients in our time together. Ive mentioned some of the key members and programs of this team throughout this book, but every member of correctional health services deserves tremendous respect for the work they do. I will discuss the nursing, medical, data, and mental health services often throughout, but a few other programs deserve acknowledgment for advancing our mission to document and reduce the health risks of jail. Our IT team in the jail correctional health service, led by Rick Stazesky, enabled us to simultaneously deliver care and capture data to detect abuse. Without this team, we could not have conducted most of our reports on health outcomes. Tom Hayden and his pharmacy team probably have the most objective and total view of the jails because of their ability to work in clinics; to monitor small, remote pharmacy windows; and even to bring medications to housing areas.
There have been several outside partners in our work who left before I did. The first is the former Department of Correction (DOC) deputy commissioner Erik Berliner. Erik was my counterpart at DOC, and we more or less came up the ranks together. His unit of DOC, called Health Affairs, existed to coordinate with us in the health unit on the many issues we shared, such as patient production, clinic productivity, and staff squabbles. I sometimes describe Health Affairs as the curtain to our tennis ball, there to soak up our kinetic energy without disturbing the security leaders. When he left the DOC about two years ago, we lost a true partner to our health service. He wasnt able to effect change in DOC on some critical issues, but he and I shared a strategic plan on how to cooperate most of the time and work around each other when we couldnt find common ground. He deserves as much credit as anyone for design of the clinical alternatives to solitary confinement units that would allow us to remove seriously mentally ill patients from solitary. Even when our agencies were headed for conflict, we had an open line of communication that helped limit harm to patients and staff.
Another partner I need to acknowledge is Cathy Potler, who was executive director of our oversight board before she passed away. Cathy was the most zealous and unapologetic advocate for our patients whom I encountered during my time in the jails. She worked tirelessly to steer her oversight body toward a more active role in holding DOC and us in correctional health accountable for compliance with basic laws and rules. During my time as medical director and assistant commissioner, she and I worked very closely to document abuse of patients and strategized how best to proceed on almost every case we encountered. Her requests for information and accountability by DOC would irritate and then anger an entire agency. Ultimately, DOC began to spend considerable amounts of time complaining to city hall about Cathy and her requests for basic data and explanations of practices. Cathy had already developed an entire career in promoting human rights, and with the staunch support of her son and husband, she seemed unaffected by the pushback from DOC and city hall. Dr. Bobby Cohen was (and remains) a member of the oversight board that Cathy led. Bobby has also been a longtime mentor to me, and for several years Bobbys and Cathys voices were quite alone, as a chorus of other NYC officials would proclaim that things were fine or improving in the jails. Had those same officials spent less time trying to marginalize Cathy, Bobby, and others raising the alert, Rikers might be closed today. About a year before her death, I brought Cathy a bottle of wine to celebrate some hopeful test results about her cancer. I was so struck that in the face of life-threatening illness she wouldnt give one inch to the system that worked so hard to marginalize her and harm the incarcerated.
There are a host of others whom I will acknowledge in the pages that follow. Ive been very fortunate to have great bosses, each of whom helped me to advance this mission at critical times and protect me at others. Maria Gbur recruited me to come be her deputy right out of fellowship, and she was a fierce and feared advocate for patient care. Louise Cohen, Amanda Parsons, and Sonia Angell were my bosses as deputy commissioners at the NYC Department of Health and Mental Hygiene, and they all gave me great support in establishing the human rights framework to correctional health. They also taught me a tremendous amount about their areas of expertise, including primary care, information technology, and chronic disease management. My recent boss at NYC Health + Hospitals, Patsy Yang, has been a tireless advocate for increasing the funding and scope of services of correctional health, and she will be a zealous guardian of our resources in coming years. Ive been able to manage the tougher stretches of this work thanks to some close and insightful confidants, including Ross MacDonald and Cecilia Flaherty, our chief of medicine and director of programs, respectively.
Our mission has also benefited from the counsel (and criticism) of groups outside correctional health, namely, a crew of progressive city council members whom I will mention later in the book, advocates like Jennifer Parrish at Urban Justice, and prisoners rights lawyers such as Dale Wilker, Sarah Kerr, John Boston, Riley Evans, and Jonathan Chassan.
My early thoughts about the health risks of jail were really influenced by quarterly meetings we set up called the Human Rights Collective. We would invite academics, professionals, advocates, and people with lived experience of incarceration to discuss difficult issues like solitary confinement, sexual violence, or racial disparities in care and punishment. These partners would teach us about some of the grim realities at play in the jails that had a major impact on the health of our patients and our ability to deliver ethical care. At one of these meetings, we started to dig into the problem of tracking and reporting abuse much more comprehensively, and a longtime research mentor, Dr. Ernie Drucker, commented that jail exposure was like being dipped in acid and then being put back in the community. This idea, along with the many partners we met with from outside our health service, helped me to appreciate the deadly and long-lasting health risks of jail.
Next page