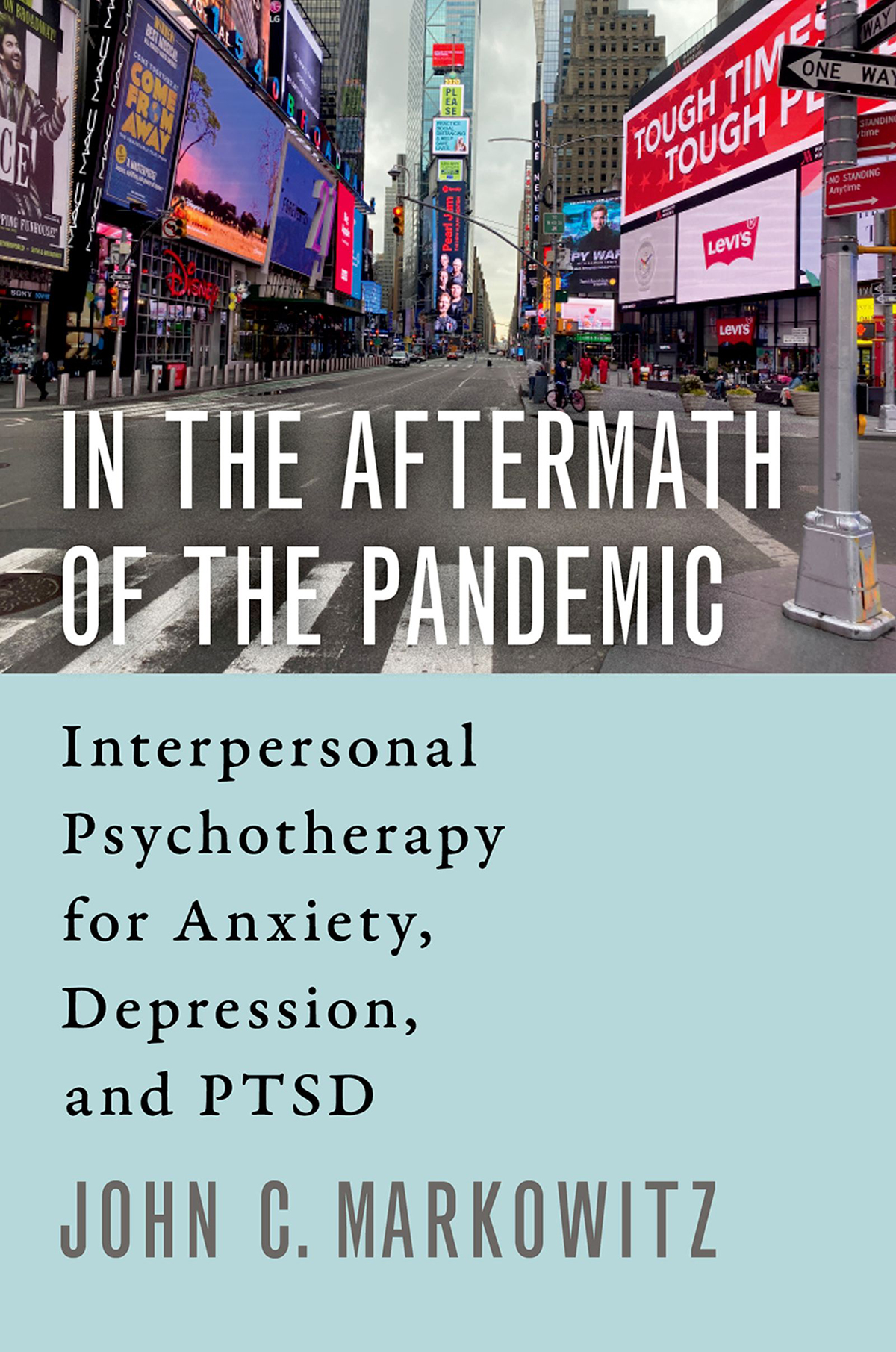
In the Aftermath of the Pandemic

Oxford University Press is a department of the University of Oxford. It furthers the Universitys objective of excellence in research, scholarship, and education by publishing worldwide. Oxford is a registered trade mark of Oxford University Press in the UK and certain other countries.
Published in the United States of America by Oxford University Press
198 Madison Avenue, New York, NY 10016, United States of America.
Oxford University Press 2021
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the prior permission in writing of Oxford University Press, or as expressly permitted by law, by license, or under terms agreed with the appropriate reproduction rights organization. Inquiries concerning reproduction outside the scope of the above should be sent to the Rights Department, Oxford University Press, at the address above.
You must not circulate this work in any other form and you must impose this same condition on any acquirer.
CIP data is on file at the Library of Congress
ISBN 9780197554500
eISBN 9780197530375
DOI: 10.1093/med-psych/9780197554500.001.0001
Dedicated to the incomprehensible numbers of the dead, of the still living and suffering, and to those struggling to help them
Contents
In 2020 the world suddenly and seemingly irrevocably changed. The Covid-19 virus, previously unknown, often lethal, and without a treatment, began to devastate populations around the globe. In the absence of a vaccine, societies retreated to ancient patterns of plague control, namely social distancing. This physical isolation protected individuals, kept intensive care units (ICUs) from overflowing, and limited at least the speed of infectionbut at a cost.
The anti-Covid lockdown in the United States saved lives, at least in parts of the country that obeyed it. It brought with it, however, a host of problems: loss of sense of health safety, and sometimes loss of health itself; loss of daily routine, loss of social support, loss of income, often loss of job, and sometimes loss of loved ones (see psychopathology on a grand scale: anxiety, depression, traumatic stress, and substance misuse. Those who havent died or become physically ill still suffer.
In the midst of this pandemic, our team of psychiatric researchers at Columbia University/New York State Psychiatric Institute (NYSPI) sought to provide remote (virtual, phone and internet video) treatment to patients in need. Remote therapy is itself a major adjustment for therapists used to seeing patients in person.
Table I.1. Losses Due to the Covid-19 Pandemic Engender Psychiatric Symptoms
| Loss | Threat | Consequences |
| Loss of security | Potentially lethal viral infectionFrontline medical and other personnel witness trauma | Fear of or actual illness anxiety, pain, PTSD, depression, anxiety |
| Loss of income | Anxiety about rent, food, finances | Anxiety, depression |
| Loss of employment | Damage to career, income | Anxiety, depression |
| Loss of loved ones | Complicated mourning | Traumatic loss; disrupted mourning rituals anxiety, depression, PTSD |
| Loss of routine | Home lockdown | Disrupted social rhythms, activities, pleasures anxiety, depression |
| Loss of social support | Physical distancing can mean social isolation | Social isolation anxiety, depression |
A further layer of interpersonal malignity magnifies the effects of coronavirus. From the start of the pandemic, Americans have seen other countries, led by unifying, compassionate leaders, take orchestrated, scientifically driven steps to combat the spread of infection, with often beneficial results. In contrast, the U.S. federal government has been divisive, attacking, openly racist at a moment when racial and ethnic minorities are hardest hit, and strikingly anti-scientific. The President of the United States has recommended unproven and dangerous remedies such as injecting bleach (!) and turned wearing a mask into a political statement rather than a public health measure. The federal and many state governments have failed on many levels, for many people, their leaders pointedly ignoring and discounting a rising plague in defiance of basic medical tenets. Spike Lee made the point in his 2006 film When the Levees Broke that although Hurricane Katrina was an impersonal trauma, the failed, racist governmental response to the disaster gave it added interpersonal insult.
Amidst the pandemic, in the anticipation of a polarized national election, there has been a sudden explosion of national awareness and protest about structural racism following airings of videotaped evidence of the killings of George Floyd on May 25, 2020, and other African American men and women, by white policemen. The Black Lives Matter movement is a healthy, belated response to centuries of inequality and mistreatment, and its invigoration seems a healthy channeling of the frustrations of months of lockdown into an idealistic cause. Dealing with structural racism is an important cause, albeit not the focus of this book. Nonetheless, all this change adds to the turmoil in the environment individuals face.
Moreover, this is only the first wave of virus, and first aftershock of psychiatric symptoms. If there are future waves, as it appears there may well be, they will likely compound the psychiatric sequelae. What effect will this pandemic have not only on the adults who lose their jobs, but also on their children who are evicted from their schools and separated from their friends for months on end? Even after a vaccine arrives, the psychiatric consequences of this global disaster will likely be long-lasting.
This book describes the application of interpersonal psychotherapy (IPT) to treating the psychiatric consequences of Covid-19, and more generally to any terrible social disaster. IPT is one of many psychotherapies, and it is surely not the only route to treating post-Covid psychological symptoms, but many therapists and patients may find it a particularly useful approach. I will explain why in a moment.
Most books on IPT have followed a research data stream. Almost every IPT adaptation for a particular psychiatric disorder has been empirically tested and shown to work before it has been disseminated. We know that IPT benefits people with major depressive disorder (MDD), will recognize the need for immediate clinical trials as a result of the mental health fallout of the pandemic. Nonetheless, as we await research evidence, IPT appears to be a good candidate for the psychiatric consequences of disaster. All of the treatment cases described in this book, while disguised to protect patient confidentiality, are actual presentations from the pandemic.
Why should IPT work in the setting of disaster? First, IPT has been shown to alleviate MDD and PTSD, two of the most common sequelae of traumatic life events, and to lower anxiety. Second, IPT is a life eventbased therapy, using life circumstances to contextualize psychiatric crises, explain strong emotional reactions, and use understanding of those emotions to negotiate interpersonal and other life difficulties.) can help to restore the lost structure of pre-Covid daily life.