Coronavirus basics
What is COVID-19?
As the pandemic evolves, sometimes we lose sight of fundamental facts that are helpful. Coronaviruses are not new. Coronaviruses were discovered in the 1960s and are one of the most common causes of colds, accounting for 20-30%. The name coronavirus comes from the way each individual virus looks under electron microscopy, with a halo similar to the corona of the sun.
Specifically bad strains of coronaviruses have caused epidemics before Middle Eastern Respiratory Syndrome (MERS) and Sudden Acute Respiratory Syndrome (SARS). This is why some vaccine efforts arent starting from scratch. These viruses stopped spreading before vaccine development could be completed. Subsequent funding and prioritization of vaccine efforts waned. But communities closer to where MERS and SARS hit were more prepared for containment efforts.
From a parenting perspective, I dont think its worthwhile to spend too much time considering where the virus originated. This strain, SARS-CoV-2, or COVID-19, is different from coronaviruses that previously circulated every year. Its novel most of us dont have protection based on prior illness, and we are still learning specifics about the virus.
The timeline of spread seems pretty settled the virus began to spread in Wuhan, China, around November 2019. The spread started small clusters of infection in more and more places until it hit NYC hard in March 2020. From NYC it has now spread all over the US.
So lets talk about what we need to know as parents. While some of the following is pretty technical, I think it provides a helpful context for the more practical advice later in the book. But if you find it too dry, skip ahead; you can always refer back to it later on.
How does it spread?
I believe that news and major health organizations have vacillated too much on this topic. The evidence seems clear that the primary route of spread in the community is by droplet, so lets dig in to learn what that means.
In all hospitals, we consider which precautions are necessary to protect both patients and staff. Particularly in the winter in childrens hospitals, we take great care to make sure children admitted after a surgery are not roomed with a child with an infectious reason for admission, like influenza. In a hospital setting, in accordance with the CDC recommendations, we think of contact, droplet, and airborne transmission.
Infections spread by contact transmission can be either direct or indirect. A direct contact spread would be from an animal bite, touching someone with scabies, or touching a herpetic lesion. The pathogen jumps over and causes damage. Indirect contact occurs through an intermediate object. If a doctor doesnt wash hands well, he or she may carry pathogens such as the bacteria that cause skin infections or infectious diarrhea from one patient to the next.
Droplet transmission is a variant of contact transmission, as most illnesses spread by infected droplets can also be spread by direct or indirect contact. Respiratory droplets are emitted when someone who is infected coughs, sneezes, or talks and can carry the pathogen to the respiratory tract or mucous membrane (i.e. eyes, nose, mouth) of others near them. Lots of common infections are transmitted this way for example, pertussis (whooping cough), influenza, rhinovirus, and strep throat. To protect yourself from droplets, distance and regular surgical masks are effective, particularly when coupled with hand hygiene.
Other illnesses, like measles, chicken pox, and tuberculosis, are airborne. That means tiny droplet residue can survive and remain in the air for longer periods of time. Air currents may lead to infection even in those who have not had face-to-face contact with an individual infected with one of these pathogens. Airborne precautions require more serious interventions typically rooms with special ventilation systems in the hospital to prevent spread. N-95 masks, which trap smaller particles than the surgical mask, are necessary for healthcare personnel exposed to these infections.
COVID-19 seems to be a hybrid. In typical settings outside a hospital or clinic, infected individuals produce droplets as many as a thousand a minute while speaking loudly without a mask. The infectious dose of COVID-19 how many viral particles are required to get sick is unknown but is estimated to be between 750 and 1,000, similar to that of the flu and other coronaviruses. However, in some situations, such as when inserting a breathing tube or doing a deep swab of the nose, some of the virus may be aerosolized and persist in the air for longer periods of time. It seems likely that activities like singing or shouting may increase the risk of generating aerosols.
This is important as we make plans to protect ourselves. Masks and hand hygiene are the cornerstones of decreasing risk of transmission. Adequate ventilation is likely to be protective, too.
What are the symptoms?
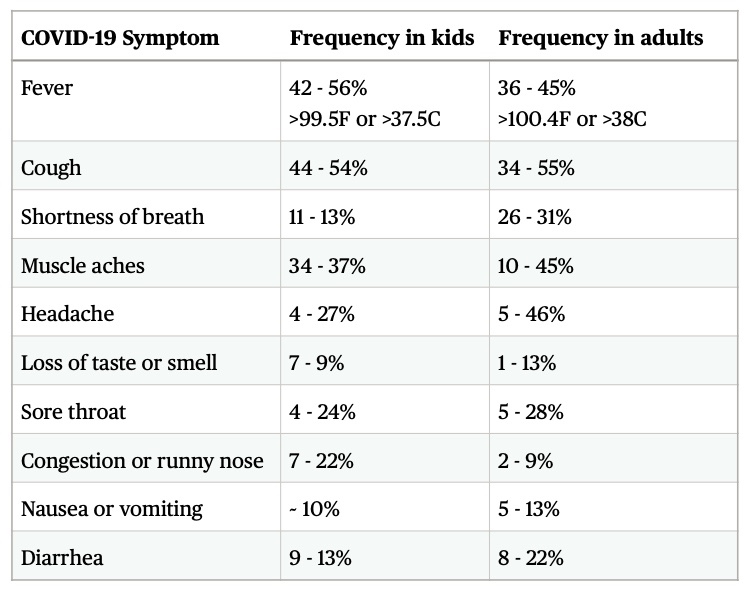
As a parent, the symptoms and signs of coronavirus infection are the most important thing to know. If someone in your family has these, its time to contact your doctor to consider testing. We re still learning about COVID-19, but the consensus is that the most common symptoms include the following.
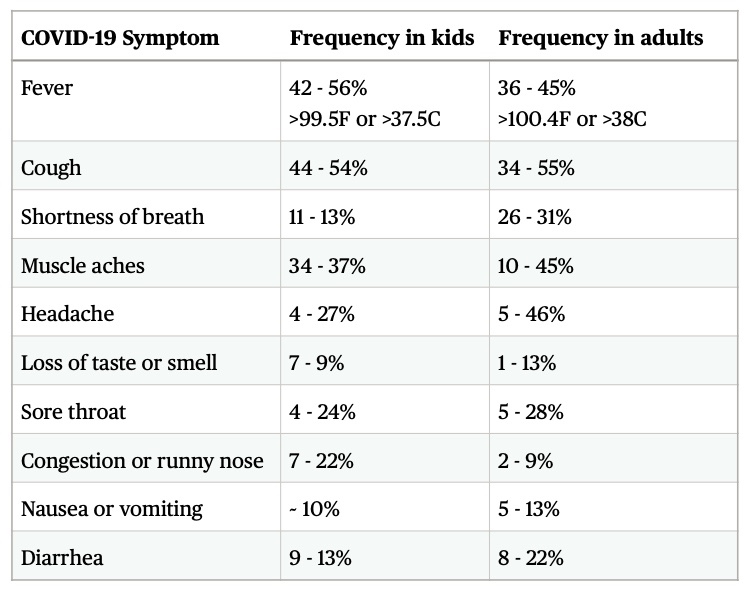
Because of limitations in testing early on, its important to emphasize these percentages are out of people who are sick and seek care for symptoms of coronavirus. Since we know many children and adults have no symptoms, we shouldnt assume, for example, that 11% of children who have coronavirus have shortness of breath. Since we know that ~80% of children with coronavirus show no symptoms, its more accurate to estimate that 11% of the 20% who have symptoms have shortness of breath. This means that only approximately 2% of all children who test positive for coronavirus have shortness of breath.
Symptoms vary considerably by age. Fever and cough are not always present, even among those with symptoms of coronavirus. Muscle aches, headaches, sore throat, and diarrhea are frequent symptoms.
Life post-coronavirus should include a high index of suspicion . Index of suspicion is a medical term that refers to our initial impression of the likelihood of the disease. We should assume that most symptoms during this time of a pandemic may be related to coronavirus. If you dont feel well or when your children dont feel well, consider pursuing testing and reaching a diagnosis.
How is it diagnosed?
Original studies in China before a test was developed used CT scans to look for damaged lung tissue. Now we use nasal swabs or saliva samples to look for detectable virus, using a technique called nucleic acid amplification (NAA). The code for the viral protein is converted; then, using Polymerase Chain Reaction techniques (PCR), the code is multiplied to facilitate detection. Nucleic acid amplification tests are very good tests, both at identifying truly positive specimens and excluding negative specimens without the virus.
Two of the biggest limitations to the test are unavoidable no matter how good the test is. First, given the natural progression of the virus, there may not be detectable virus in an obtained specimen early on. The incubation period the time between being exposed to the virus and falling sick is about five days but may be as long as 14 days. In the pre-symptomatic stage, the day or two before you start feeling crummy, you may be transmitting the virus even though you are not showing symptoms. Even if sick, you may test negative for the first two days of feeling ill despite being potentially contagious. All of this is to say, if you get tested one day after exposure and the test is negative, that doesnt tell you if you will get or transmit coronavirus.


 Coronavirus basics
Coronavirus basics