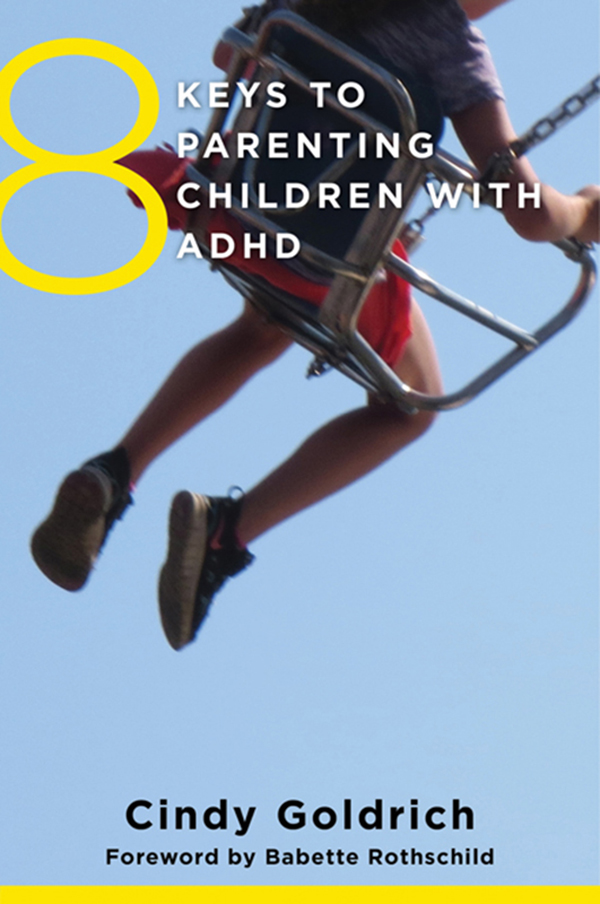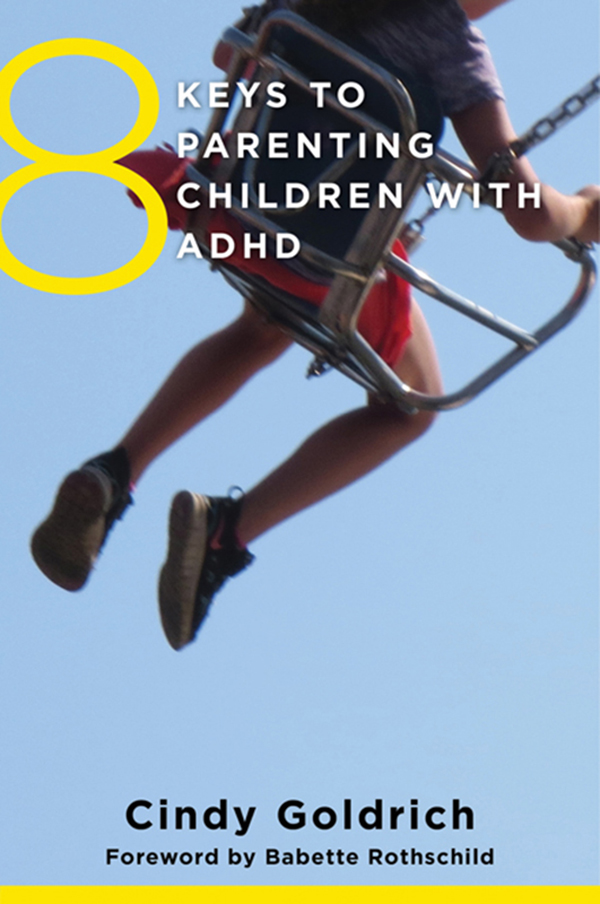
8 Keys to Parenting Children with ADHD
Copyright 2015 by Cindy Goldrich
All rights reserved
First Edition
For information about permission to reproduce selections from this book,
write to Permissions, W. W. Norton & Company, Inc.,
500 Fifth Avenue, New York, NY 10110
For information about special discounts for bulk purchases, please contact
W. W. Norton Special Sales at specialsales@wwnorton.com or 800-233-4830
Production manager: Christine Critelli
The Library of Congress has cataloged the printed edition as follows:
Goldrich, Cindy.
8 keys to parenting children with ADHD / Cindy Goldrich ; foreword by Babette
Rothschild. First edition.
pages cm.(8 keys to mental health series)
Includes bibliographical references and index.
ISBN 978-0-393-71067-0 (pbk.)
1. Attention-deficit-disordered children. 2. Attention-deficit-disordered children
Family relationships. 3. Parents of attention-deficit-disordered children. 4. Parenting.
I. Rothschild, Babette. II. Title. III. Title: Eight keys to parenting children with
ADHD.
RJ506.H9G645 2015
618.92'8589dc23
2015017869
ISBN 978-0-393-71068-7 (e-book)
W. W. Norton & Company, Inc.
500 Fifth Avenue, New York, N.Y. 10110
www.wwnorton.com
W. W. Norton & Company Ltd.
Castle House, 75/76 Wells Street, London W1T 3QT
8 KEYS TO
PARENTING
CHILDREN
WITH ADHD
CINDY GOLDRICH
FOREWORD BY BABETTE ROTHSCHILD

W.W. Norton & Company
New York London
8 KEYS TO
PARENTING
CHILDREN
WITH ADHD
Start with wherever you are with whatever youve got.
John Rohn
I f you are seeking support for parenting your child, chances are that your journey so far has been full of challenges, worries, frustrations, and perhaps even disappointments. Now is a great time to take a moment and commit to recognizing that whatever has brought you to this place, this is just where you are now. I often hear parents express guilt, concern, and confusion regarding how they have been parenting their kids. Please know this: Poor parenting cannot and does not cause ADHD; it is a neurodevelopmental disorder. ADHD is real! Although some people claim that food additives, sugar, yeast, or poor child rearing methods lead to ADHD, there is no conclusive evidence to support these beliefs (Barkley, 1998a; Neuwirth, 1994; NIMH, 1999). causative role in ADHD (personal correspondence, October 21, 2014). In fact, imaging studies show differences in the structure and activity between brains of people with and without ADHD. In people with ADHD, there is a consistent pattern of below-normal activity in the neurotransmission of the chemicals dopamine and norepinephrine in the brains prefrontal cortex (the front part of the brain). As a result of the lower levels of dopamine, there is understimulation in the reward and motivation centers in the brain. The prefrontal cortex is thinner and matures more slowly. This does not imply any deficit in intelligence or ability to succeed.
So much of what we now understand about ADHD has been learned during the past decade. Few people instinctually know how to handle the atypical behavior we see in kids with ADHD. Unfortunately, most teachers and a significant number of therapists, pediatricians, and psychiatrists have not been formally educated about the academic, social, and emotional impact ADHD has on individuals throughout the life-span. Thankfully, there are many professionals who do actively seek to stay current by attending conferences and workshops and by reading scientific and research journals. It is vital that you, as your childs parent, form a team of support that includes knowledgeable experts.
When most people think about ADHD, they associate it with the main three traits of impulsivity, hyperactivity, and inattentiveness. Science and research have helped us to understand that these traits are really just the tip of the iceberg, as author Chris Dendy says. There is much more that lies beneath the surface and impacts every aspect of a persons life.
Diagnosing ADHD
While some people feel that they can easily diagnose ADHD based on simple checklists, a proper diagnosis is more complex. I recommend that you seek a professional evaluation to make sure that you are not being swayed by incomplete or inaccurate information.
One of the questions I am often asked is, Who can diagnose ADHD? The answer is not as straightforward as one would hope. While any psychiatrist, pediatrician, psychologist, social worker, or nurse practitioner can technically diagnose ADHD, I strongly urge a parent to seek out someone who is specifically trained and knowledgeable about current criteria and best practices.
There is no single, objective test available to definitively diagnose ADHD. A comprehensive evaluation is necessary to make a proper diagnosis, as well as to determine if there are any coexisting conditions. An accurate diagnosis must include:
An in-depth clinical history of both the child and the family.
A physical exam to help rule out other possible causes of symptoms (e.g., sleep apnea, thyroid condition).
A clinical assessment using standardized behavior rating scales or questionnaires. These forms may be completed by the childs teacher, the childs parents, or in some cases the child himself or herself. There are several respected rating scales in use today, including Conners Rating Scale, the Vanderbilt Assessment Scales, and the Barkley Home and School Situations Questionnaires.
An evaluation of the childs intelligence, aptitude, personality traits, or processing skills.
A complete neuropsychological or educational exam is not always necessary. If there are any concerns about learning or processing, however, I generally do recommended full testing. A neurological assessment that includes screenings of vision, hearing, verbal, and motor skills may also be recommended.
Parents are often surprised and comforted when they realize that many of the behaviors they observe in their child can be attributed to the neurobiology of ADHD. Having a complete picture of your child will help you, and your child, effectively understand and manage the challenges he or she faces as well as the strengths he or she can call upon.
What Is ADHD?
First off, some clarification: Until 1994, what we currently call ADHD was known as attention deficit disorder (ADD). Many still refer to it that way, especially when trying to distinguish whether a person has the hyperactivity component. However, as you will see, this is technically incorrect. Sadly, before 1968, this disorder was referred to as minimal brain dysfunction or minimal brain disorder. Whereas previous editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM) used by health care professionals to diagnose mental disorders included three subtypes of ADHD, the current DSM-5 now distinguishes the categories as three presentations:
ADHD Hyperactive/Impulsive
ADHD Inattentive
ADHD Combined Hyperactive/Impulsive and Inattentive
A person can change presentations during his or her lifetime, as we often see a reduction in hyperactivity as an individual grows.
There is now a fourth category that is highly related to ADHD, although at this point researchers are still exploring whether this is a separate condition or part of ADHD itself. Concentration deficit disorder
Next page