Table of Contents
List of tables
List of figures
Landmarks
Acknowledgements
We owe a prodigious amount of thanks to key individuals without whom this third edition would not have been completed. Claire Wanless created the new design and her editorial guidance has been masterly and absolutely invaluable. Philip Wilson produced the exquisite drawings that are a key part of each and every chapter. Jeremy Weldon, Consultant radiographer at Northwick Park Hospital helped us with the illustrative cases and he carried out the laboratory work on penetrating and swallowed foreign bodies. Dr Denis Remedios, Consultant radiologist at Northwick Park Hospital provided many original suggestions. Michael Houston, senior commissioning editor at Elsevier Ltd, prompted us to produce this third edition and facilitated and assisted us in our endeavours.
Our thanks are also due to a large and anonymous group, comprising doctors, radiographers, and radiologists in training who have attended our courses (www.radiology-courses.com and www.xraysurvivalguide.org), and through their constructive feedback have stimulated us to enhance numerous aspects, both large and small, in every chapter.
That is the essence of science:
ask an impertinent question and you are on the way to a pertinent answer.
J. Bronowski, The Ascent of Man, 1973.
Test Yourselfanswers
.
.
.
.
.
.
.
.
.
; an intra-articular fracture is not evident on this single view, but is presumed to be present.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Key principles
Introduction
Patients with traumatic injuries can be placed into one of three major groups. The imaging approach will differ between these groups.
Polytrauma (in which one injury may be life threatening)
Imaging:
.
Multiple injuries (none of which is life threatening)
Imaging:
Plain film radiology is utilised in the ED.
Single injury (not life threatening)
Imaging:
Plain film radiology is the principal imaging investigation.
This book describes the assessment and interpretation of the plain radiographs that are customarily obtained in patients who have not sustained a life threatening injury.
Basic radiology
The radiographic image
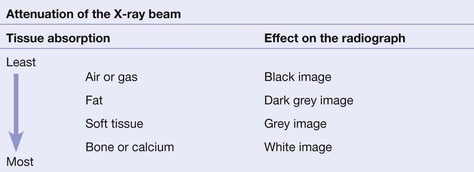
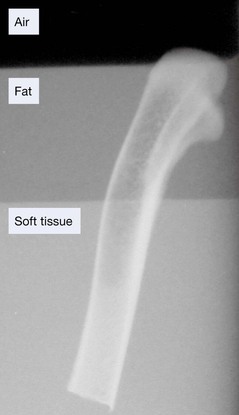
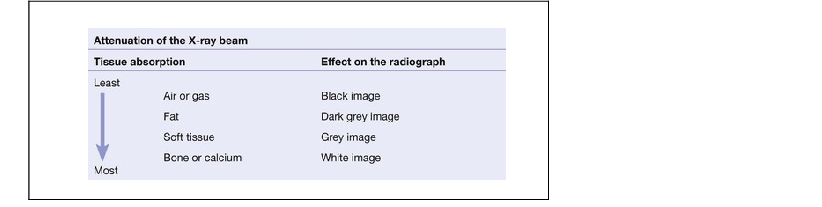
The tissues that lie in the path of the X-ray beam absorb (ie attenuate) X-rays to differing degrees. These differences account for the radiographic image.
Radiograph of a chicken leg (bone) partially submerged in a layer of vegetable oil (fat) floating on water (soft tissue). Note the difference in the blackening of the X-ray film due to absorption by the different tissues.
Fracture lines: usually black, but sometimes white
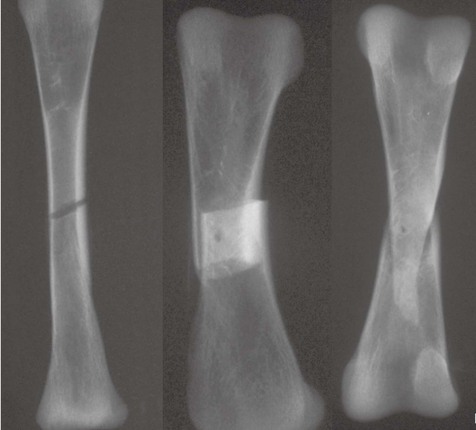
When a fracture results in separation of bone fragments, the X-ray beam that passes through the gap is not absorbed by bone. This results in a black (ie lucent) line on the radiograph.
On the other hand, bone fragments may overlap or impact into each other. The resultant increased thickness of bone absorbs more of the X-ray beam and so results in a white (ie sclerotic or denser) area on the radiograph.
Three fractures. On the left the fragments are distracted and the fracture shows as a dark black line. In the centre the fragments overlap resulting in a dense region on the radiograph. On the right the fragments are impacted, also producing a dense region.
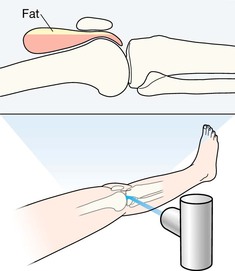
Fat pads and fluid levels
There are radiological soft tissue signs which can provide a clue that a fracture is likely. These include displacement of the elbow fat pads (see ).
The principle of two views
One view only is one view too few
Many fractures and dislocations are not detectable on a single view. Consequently, it is normal practice to obtain two standard projections, usually at right angles to each other. The example below shows two views of an injured finger.
At sites where fractures are known to be exceptionally difficult to detect (for example a suspected scaphoid fracture), it is routine practice to obtain more than two views.
Injured finger.
The true extent of the injury is only evident on the lateral view.
Important information: patient position
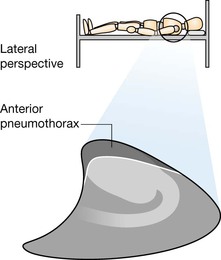
Knowledge of the patient's position during radiography is essential. A radiograph obtained with the patient lying supine may produce a very different appearance when compared with the image acquired with the patient erect.
Example 1.
Injured knee. Patient supine. A fatfluid level in the suprapatellar bursa () will only be seen when the radiograph is obtained with a horizontal X-ray beam. A vertical beam radiograph will not demonstrate the fatfluid level.
Example 2.
A small pneumothorax will usually be detectable at the apex of the lung on an erect chest X-ray (CXR). On a supine CXR you need to look much lower down, ie around the heart, the diaphragm, and at the costophrenic angle.
Assessing the radiographs: discipline is essential
Missed injuries are common following trauma. Detection of a fracture, and the components of a complex injury, depends on adherence to three cardinal rules:
Rule 1 . Always analyse both views.
Rule 2 . Develop a systematic step-by-step checking process for each radiograph even if a single abnormality is obvious. Two associated abnormalities often occur. The major danger: you can be seduced by the satisfaction of search phenomenon (YesI have found the abnormality! ), and consequently a second important abnormality is overlooked.
.
Describing injuries
Fractures of the long bones
The radiographic appearance of a fracture needs to be described in a consistent style using accepted terminology. Imagine that you are describing a fracture of a long bone to the surgeon over the telephone. These are the features the surgeon will want you to describesimply and accurately:
Site .
Closed or open.
Fragments .
Direction of the fracture.
Articular surface involvement .


![William Herring - Learning Radiology: Recognizing the Basics [with Student Consult Online Access]](/uploads/posts/book/310283/thumbs/william-herring-learning-radiology-recognizing.jpg)