A tibial pilon fracture is a bony lesion that involves the distal meta-epiphyseal tibia associated with an important cartilage involvement [].
These injuries represent about 1% of the lower limb fractures [].
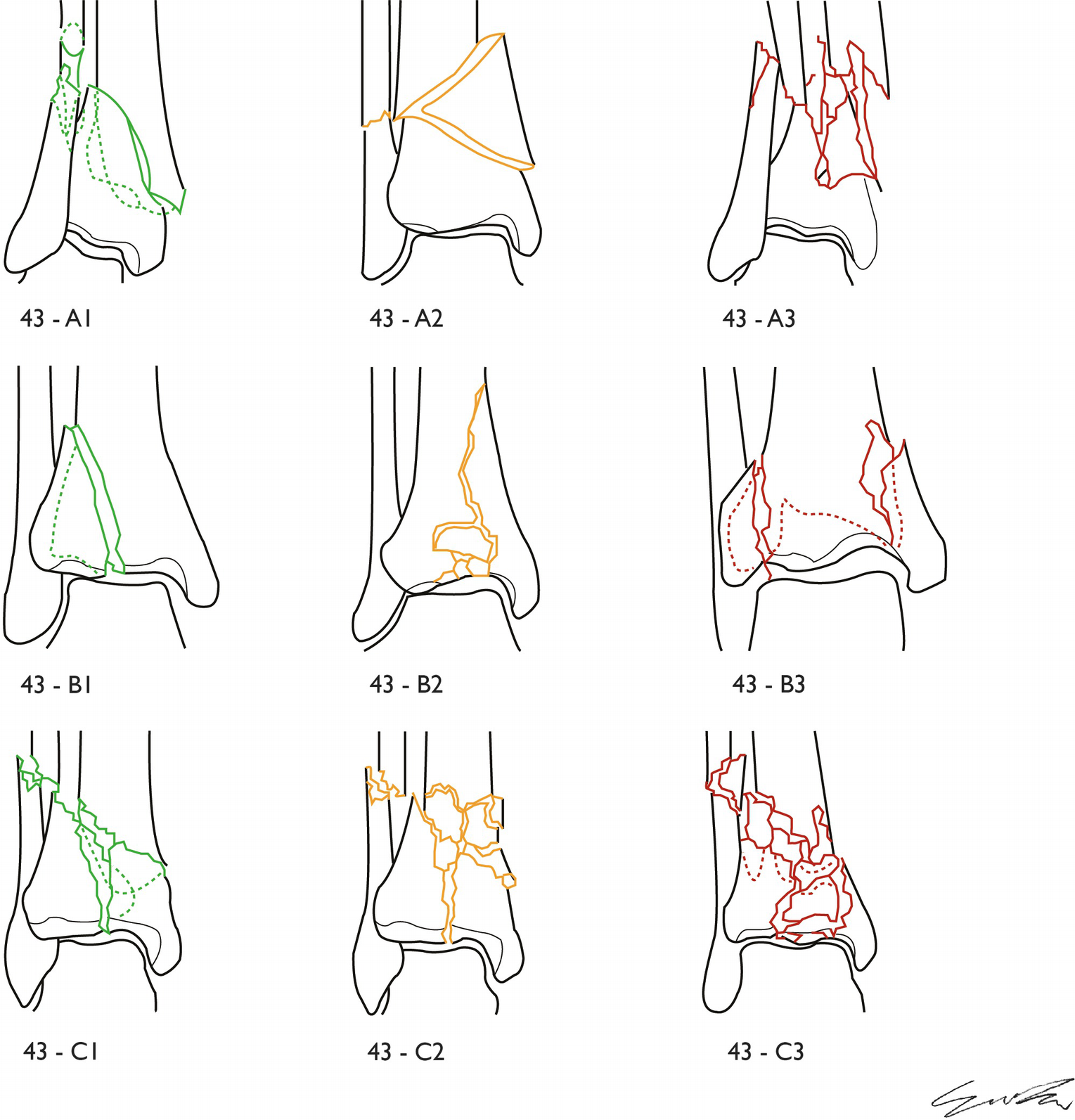
1.1.1 Classification
According to the AO classification [). The latter are the more properly defined tibial plafond fractures, and it is useful to further divide them in subgroups regarding their comminution: C1 if there are only big fragments and there is no comminution, C2 if there is only comminution of the extra-articular metaphyseal part and C3 if there is comminution of both articular and extra-articular components.
Fig. 1.1
AO classification of the distal tibia epiphysis fractures; subgroup A indicates the extra-articular fractures, B subgroup the partially articular fractures and subgroup C the fractures of the tibial pilon, in which the joint involvement is complete with an entire separation between the diaphysis and the joint part
Such subdivision is not only descriptive, but it is related to the traumatic mechanism that generates the fracture, usually a low kinetic energy event with mainly torsional stress in the less comminuted fractures and high energy event with mainly compressive stress in the more comminuted cases [].
Since during the fracture evaluation it is possible to encounter borderline cases regarding the fragmentation and the correct definition of the comminution, practically the fracture is assigned to the C2 and C3 categories, with high complexity features, only if there are one or more fragments halfway the main ones, and it is not possible to obtain a complete contact between the latter even after the fracture reduction [].
1.1.2 Treatment and Indications
Being articular fractures, the ideal treatment should be the anatomical reduction and stable internal fixation, to reduce the arthritic joint degeneration through a precise reconstruction of the joint surface and to allow early joint mobilization, aiming to preserve the range of motion, thanks to the protective function of the mobilization on the cartilage [].
If there is bony exposition and soft tissue loss of substance, it is convenient to proceed if possible before 24 h from the injury with an external fixator positioning and through the debridement of the soft tissues [].
It is advisable during this procedure to irrigate the wound with saline solution to facilitate the removal of foreign bodies and to reduce the bacterial concentration [].
The closure of the wound during the acute phase is associated with a high risk of complications, and it is advisable to consider the use of interrupted stitches or to delay the wound closure, through second intention healing, that becomes imperative in the more severe wounds, in which the use of a skin graft can be necessary.
The use of vacuum-assisted closure (VAC) has a key role to obtain the best results when plastic surgery is needed and more broadly to obtain the best healing for the soft tissues [].
The antibiotic therapy with first-generation cephalosporin, begun within 3 h from trauma, is proven to reduce significantly the infection rate of open wounds [].
Even closed injuries require a treatment specifically orientated in the management of the extra-osseous anatomy: around the ankle there is a poor representation of soft tissues, and there are no muscles that protect the deep planes; for this reason there is a dangerous and precarious biology that highly exposes to complications an open reduction and internal fixation procedure [].
To avoid such risk, the more effective strategy appears to be a staged treatment [].
Because the time window in which the soft tissue stabilization is achieved and the open reduction and synthesis are possible is brief, it seems to be advisable to establish a trauma management protocol that considers all the variables and helps the surgeon to choose the more appropriate moment to take the decisions regarding the indications.
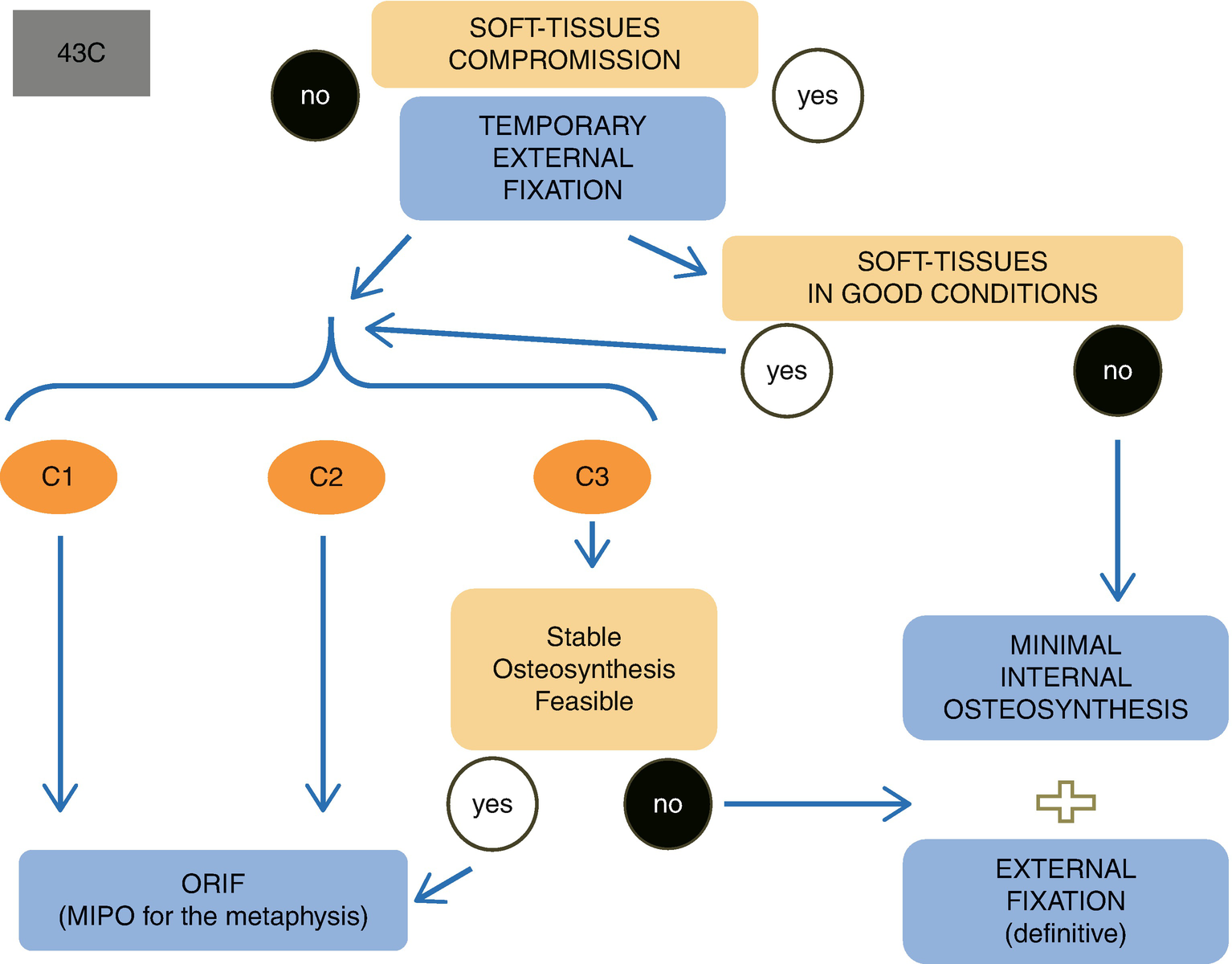
An example of this protocol, concerning complete articular fractures (AO 43C), is depicted in Fig. ].
Fig. 1.2
Example of decisional procedure that takes care of the complete joint fractures of the tibial pilon (43C considering the AO classification)
After a waiting and clinical supervision period, reported in literature as a minimum of 4 days and maximum of more or less 14 days from trauma [].
The same considerations are valid for the partial articular and the extra-articular fractures (43B and 43A), normally more simple to synthetize but equally exposed to soft tissue problems.
1.1.3 Temporary Stabilization
1.1.3.1 Goals
The objective is to neutralize the stress on the soft tissues derived from the loss of continuity induced by the fracture and the consequent hematoma induced by the bone bleeding.
This is achieved through the bridge distraction obtained with an external fixator, roughly realigning the bony segments by the traction of the capsular and ligamentous components.
The aim is to gain a sufficient stability that reduces fracture bleeding and allows the non-bearing position manageable by the patient, creating the best conditions for the unswelling of the soft tissues, necessary to facilitate the next surgical steps.
The external fixator positioning necessary to achieve these objectives must not jeopardize the future surgical options.
If trans-skeletal tractions are avoided, the patients nursing is easier, with a more simple mobilization for the hygiene, and if the skin conditions are not seriously compromised, it is possible to discharge temporarily the patient before the final surgery.
Furthermore the possibility to perform a CT scan with the bony fragments distracted and realigned is essential, because it permits a better interpretation of the fracture characteristics and personality, allowing a more simple and reliable final surgical planning.
1.1.3.2 Surgical Technique
All the configurations of the external fixator must have the screws positioned without interfering with any vascular, nervous, tendon and muscular structures and distant from the planned skin incision to avoid contamination of the surgical access [].
Considering such external fixation as a portable traction, namely, a pure temporary stabilizer, to leave in site only for a few days before the definitive osteosynthesis, it is possible to reduce at minimum the fixation elements and exoskeleton and consequently minimize the surgical aggression, allowing the use in a normal emergency room, with a simple sedation and without the use of X-rays [].