Maculopapular Drug Eruption
Maculopapular eruption, also known as morbilliform eruption or exanthema, is the most common type of cutaneous drug reactions. It is characterized by small, distinct, bright-red maculopapular lesions with a symmetrical distribution. The eruption often shows a morbilliform pattern resembling measles, but unlike measles and other viral eruptions, which characteristically starts on the face, it usually starts on the trunk, subsequently involving the face and the extremities (Figs. ). The eruption might have a purpuric character on the lower extremities. In rare cases, it may evolve into erythroderma/exfoliative dermatitis.
Fig. 1.1
Maculopapular/morbilliform drug eruption on the trunk and upper extremities showing confluent lesions on the abdominal skin
Fig. 1.2
A close-up of confluent maculopapular lesions on the abdominal skin shown in Fig.
Fig. 1.3
Maculopapular drug eruption on the trunk and upper extremities including the dorsum of the hands
Fig. 1.4
Maculopapular drug eruption on the back skin showing confluence of the lesions
Fig. 1.5
Maculopapular drug eruption on the outer part of the upper arm and the back skin
Fig. 1.6
Maculopapular drug eruption involving the palms
Maculopapular drug eruption might be accompanied by a mild pruritus. Fever and systemic symptoms are usually absent.
Histopathology shows perivascular lymphocytic infiltration with or without eosinophils with minimal epidermal changes [].
Beta-lactam antibiotics such as amoxicillin and ampicillin are the main inducers of this type of drug eruption. Cephalosporins, antiepileptics, sulfonamide antibiotics, and allopurinol may also be frequently associated with maculopapular drug eruption []. The eruption usually starts within a few days to a few weeks of drug therapy. Ampicillin-induced exanthema in patients with infectious mononucleosis might be regarded as a prototype of this eruption. Regarding cardiovascular drugs, maculopapular eruption is seen with angiotensin-converting enzyme inhibitors (ACEIs) (mainly captopril), angiotensin II receptor blockers (ARBs), calcium channel blockers (CCBs), class I antiarrhythmics, diuretics, platelet inhibitors, and aminocaproic acid.
Differential diagnosis should include viral exanthemas and syphilitic roseola. Viral exanthema characteristically starts from the face, and it is usually associated with fever and enlarged lymph nodes. Syphilitic roseola are rich on spirochetes.
Cessation of the causative drug and treatment with topical corticosteroids, systemic antihistamines, and if necessary systemic corticosteroids usually result in recovery of the condition.
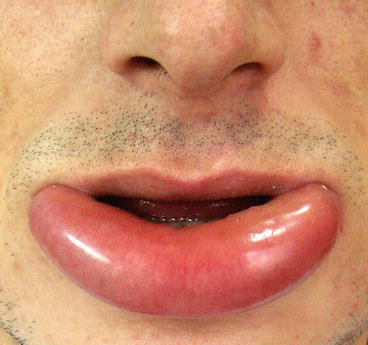
Drug-Induced Angioedema/Urticaria
Urticaria is the second most common type of cutaneous drug reactions that is characterized by sudden occurrence of red to pale itchy wheals (Fig. ), eyelids, tongue, or genitalia as deep urticarial papules and plaques. Acute anaphylaxis, and anaphylactoid reactions typically present with angioedema, urticaria, dyspnea, and hypotension.
Fig. 1.7
Pale, itchy wheals with erythematous borders on the neck in urticarial drug eruption
Fig. 1.8
Skin angioedema presenting as deep urticarial papules and plaques on the trunk
Fig. 1.9
Angioedema of the lower lip
Histopathology of drug-induced urticaria is usually consistent with classic urticaria, showing vasodilatation and dermal edema and perivascular lymphocytic infiltration occasionally with a few eosinophils [].
Drug-induced urticaria may be immunologic or non-immunologic. The main inducers of an immunologic urticaria that is frequently associated with type I hypersensitivity reaction are beta-lactam antibiotics. Immunologic urticaria might also be associated with type III hypersensitivity. The main inducers of non-immunologic drug-related urticaria include acetylsalicylic acid, other NSAIDs, radiocontrast media, opiates, and ACEIs. According to a meta-analysis, there is also risk of angioedema with ARBs in patients with prior angioedema associated with ACEIs [].