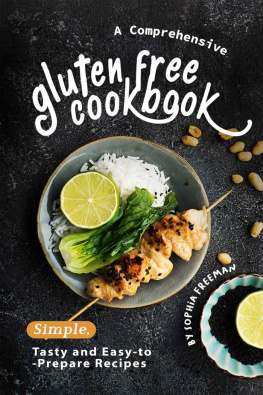
chapter one
who needs a gluten-free diet?
There are two kinds of people who need to be on a gluten-free diet. One is the coeliac (celiac) and the other is the gluten allergic. The two are completely different conditions although they are often confused with one another.
coeliacs
Up to the middle of the 20th century, the coeliac condition could prove fatal as a gluten-free diet was not used and medicine, drugs or surgery were not the answer. However, it was discovered that a gluten-free diet could control the illness, and today the outlook for the coeliac is good, providing the gluten-free diet is strictly adhered to. Any lapses, however small, can result in a setback with return of symptoms. The diet is for life in more ways than one.
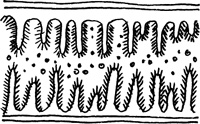
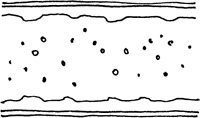
In coeliacs, the small intestine is affected. This is situated between the stomach area and the large intestine, in the lower part of the abdomen. By the time food reaches the small intestine, half way down the food canal, it is ready to be absorbed into the bloodstream. Any waste food is sent on down to the large intestine. The small intestine has a special lining of little fronds (villi). Each frond is covered in tiny hairs (the brush border). As the food, already processed, passes down the small intestine, the villi and the brush border absorb the nutrients from the food. Unfortunately, in coeliacs, gluten in the food causes the villi to shrink and become quite flattened. The food passes through and fails to be absorbed. This causes unpleasant symptoms and the coeliac becomes malnourished. The patient looks and feels completely washed out not surprising in the circumstances.
Changes in small intestine in the coeliac (celiac) condition.
Normal
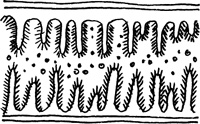
Villi with brush border and particles of food for absorption and digestion.
Abnormal
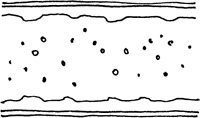
Villi flattened so particles of food cannot be absorbed and digested.
The coeliac condition is a puzzling one to diagnose as the patient seems to eat well but not to thrive. In the case of the coeliac child, there can be failure to grow, and the more the child eats the worse the condition becomes as more gluten is consumed. But there is good news: without gluten in the diet, the damaged lining of the small intestine is able to grow back the villi and brush border. Once the function is restored, health and vitality can be regained and children can grow again.
Some coeliacs with less severe symptoms can remain undiagnosed for years and continually suffer and recover. Common diagnoses for this are a digestive disorder, irritable bowel syndrome (IBS), allergy or, worse still, imagination. When eventually diagnosed, it is sometimes called silent coeliac disease.
gluten allergy
The symptoms for food allergy/intolerance/sensitivity are many and varied. They have little or no connection with the coeliac (celiac) condition. An allergy, intolerance or sensitivity to gluten may manifest itself in one or more symptoms. It is difficult to be specific about what is causing the symptoms as they can also be caused by other factors. There is now a detection kit available from pharmacies. Consult the qualified pharmacist for advice. People with persistent symptoms should consult their medical practitioner and not try to diagnose and treat themselves.
physical symptoms
head
Feeling dizzy or faint, headaches, migraine, heavy feeling.
eyes
Watery, itchy, red, swollen, tired, sore, blurred vision, heavy feeling in eyelids.
nose
Runny nose, sneezing, itching, burning, excessive mucus, blocked nose, sinusitis.
ears
Ringing in the ears, soreness, loss of hearing, earache, burning sensations, itching.
throat and mouth
Soreness, sore gums, swollen tongue, mouth ulcers, loss of taste, hoarseness, cough, choking fits, itching of the roof of the mouth, bad breath.
heart and lungs
Chest pains, palpitations, rapid heartbeat, asthma, chest congestion, tightness across chest, shallow breathing, excessive sighing, breathlessness, catarrh.
gastro-intestinal
Nausea, vomiting, stomach cramps, diarrhoea, constipation, swollen stomach, bloated feeling after eating, flatulence, feeling full up long after meals, stomach pains, poor appetite, cravings for foods, dyspepsia.
skin
Rashes, hives, inexplicable bruises, easily marked skin, eczema, excessively pale colour, dermatitis, itching, soreness, redness, sores, acne.
other physical symptoms
Weakness, cramp, cold hands and feet, flushing, shivering fits, trembling, aches and pains in the joints, swelling of the limbs, aches and pains in the muscles, swelling of the face, hands, feet, ankles, constant feeling of hunger, gorging with food, oedema, obesity.
behavioural and psychological symptoms
Nervousness, anxiety, panic attacks, depression, apathy, irritability, day-dreaming, confusion, restlessness, poor concentration, mood swings, aggression, unreasonable giggling or weeping, speech difficulties, couldnt-care-less attitude, general feeling of misery, excessive sleeping, hyperactivity, insomnia.
attitude to a gluten-free diet
The attitudes of both the gluten-free dieter and the rest of the population are crucial concerning the diet. The gluten-free dieter is in a very small minority. The rest of the population forms a huge majority and only a tiny percentage of it has even heard of a gluten-free diet.
getting it wrong
When people feel sorry for a gluten-free dieter it is usually because they perceive the special food to be second-rate in some way and an apology for the real thing. The dieter then feels at a disadvantage and takes on the role of victim, beset with eating problems, always causing a fuss at mealtimes, a burden to the family cook, school meal cooks, family and friends. Food equals a problem, day in, day out. This is a badly managed situation. Poor so-and-so, on that dreadful diet. Disaster!
getting it right
If the special dieters food looks attractive and tastes good, is interesting and varied, the attitude of people around is quite different. They are curious, envious, want to taste the food, enjoy it and be on the side of the dieter. This makes the dieter feel special. Problems involving food preparation can be ironed out and so they fade into the background. The dieter is seen to be enjoying food and life. This is a well-managed situation. Lucky so-and-so. I wouldnt mind being on your diet. Success!
cooking skills
Children and adults should be encouraged to take an interest in gluten-free food preparation and be allowed to help in the kitchen. The skill involved is a valuable one for life. It should not be a mystery.
chapter two
cooking for a gluten-free diet
The sudden introduction of a special diet into the running of a household can be a traumatic experience. Often there is very little help available at the crucial beginning of the diet, especially if there is no dietitian to give advice. If the situation is badly handled the special dieter can unintentionally be made to feel abnormal and a nuisance. A child on a strict diet can instinctively feel he or she is a source of worry as the mealtime routine is suddenly changed.