Lee John Skandalakis , John E. Skandalakis and Panajiotis N. Skandalakis Surgical Anatomy and Technique A Pocket Manual 10.1007/978-0-387-09515-8_1 Springer Science+Business Media, LLC 2009
1. Skin, Scalp, and Nail
Anatomy
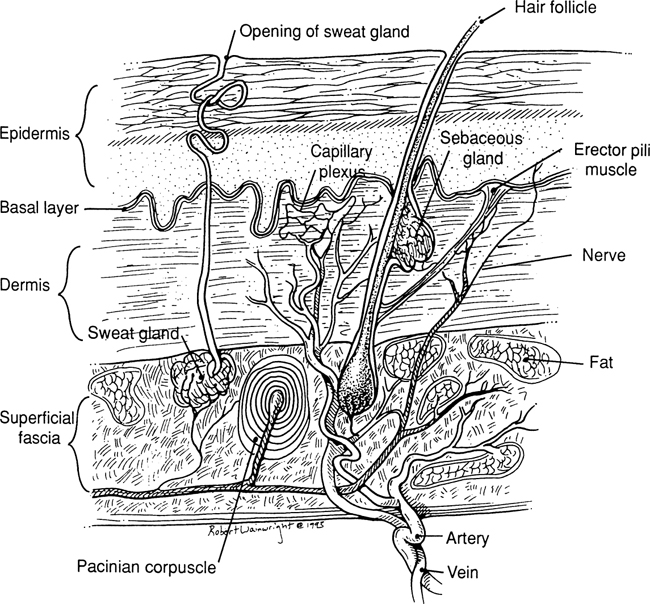
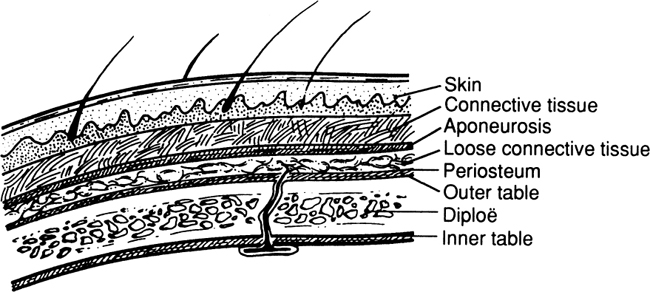
Skin And Subcutaneous Tissue (Fig. )
The skin is composed of two layers: the epidermis (superfi cial) and the dermis (under the epidermis). The thickness of the skin varies from 0.5 to 3.0 mm.
The epidermis is avascular and is composed of stratifi ed squamous epithelium. It has a thickness of 0.04 0.4 mm. The palms of the hands and the soles of the feet are thicker than the skin of other areas of the human body, such as the eyelids.
The dermis has a thickness of 0.52.5 mm and contains smooth muscles and sebaceous and sweat glands. Hair roots are located in the dermis or subcutaneous tissue.
Vascular System
There are two arterial plexuses: one close to the subcutaneous fat (subdermal) and the second in the subpapillary area. Venous return is accomplished by a sub-papillary plexus to a deep plexus and then to the superfi cial veins. A lymphatic plexus is situated in the dermis, which drains into the subcutaneous tissue.
Nervous System
For innervation of the skin, there is a rich sensory and sympathetic supply.
Remember:
The epidermis is avascular.
The dermis is tough, strong, and very vascular.
The superficial fascia is the subcutaneous tissue that blends with the reticular layer of the dermis.
The principal blood vessels of the skin lie in subdermal areas.
The basement membrane is the lowest layer of the epidermis.
The papillary dermis is the upper (superficial) layer of the dermis, just below the basement membrane.
The reticular dermis is the lower (deep) layer of the dermis, just above the fat.
Scalp
The following mnemonic device will serve as an aid in remembering the structure of the scalp. (See also Fig..)
Vascular System
Arterial Supply
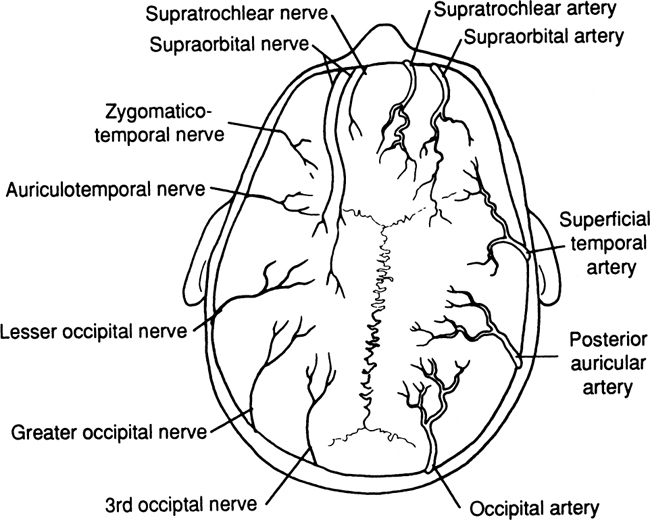
The arteries of the scalp are branches of the internal and external carotid arteries. The internal carotid in this area becomes the supratrochlear and supraorbital arteries (Fig. ). Abundant anastomosis takes place among all these arteries. All are superfi cial to the epicranial aponeurosis.
Figure 1.3.
Arterial blood supply shown on right. Nerve distribution shown on left. Veins are not shown, but follow the arteries.
Venous Drainage
Veins follow the arteries.
Lymphatic Drainage
The lymphatic network of the scalp is located at the deep layer of the dense connective subcutaneous tissue just above the aponeurosis (between the connective tissue and aponeurosis). The complex network has frequent anastomoses. The three principal zones are the frontal, parietal, and occipital.
Note:
The blood supply of the scalp is rich. Arteries are anastomosed very freely.
The arteries and veins travel together in a longitudinal fashion.
A transverse incision or laceration will produce a gap. Dangerous bleeding will take place from both vascular ends due to nonretraction of the arteries by the close, dense, connective layer.
Always repair the aponeurotic galea to avoid hematoma under it.
With elective cases (excision of sebaceous cysts, etc.), whenever possible, make a longitudinal incision.
Drain infections promptly. Use antibiotics to prevent intracranial infections via the emissary veins.
Shave 12 cm around the site of the incision or laceration.
After cleansing the partially avulsed scalp, replace it and dbride the wound; then suture with nonabsorbable sutures.
Use pressure dressing as required. Sutures may be removed in 35 days.
Be sure about the diagnosis. A very common sebaceous cyst could be an epidermoid cyst of the skull involving the outer or inner table, or both, with extension to the cerebral cortex. In such a case, call for a neurosurgeon. The best diagnostic procedure is an AP and lateral film of the skull to rule out bony involvement.
Because the skin, connective tissue, and aponeurosis are so firmly interconnected, for practical purposes, they form one layer: the surgical zone of the scalp.
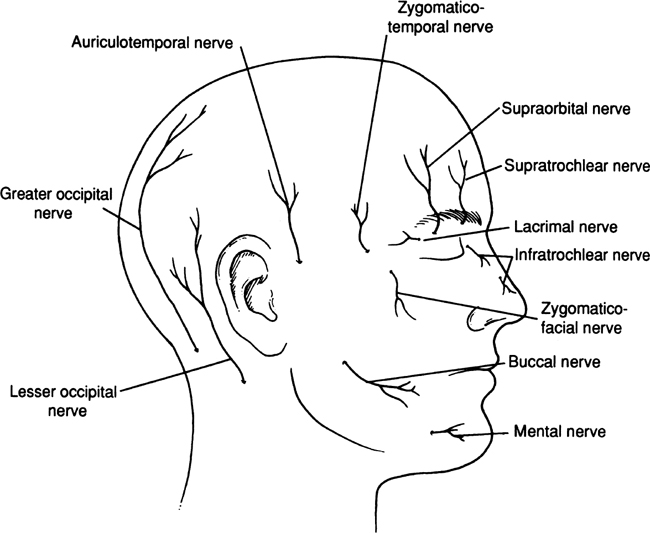
Nerves (Figs. )
The following nerves innervate the scalp: (Their origins are in parentheses.)
Lesser occipital (second and third ventral nerves)
Greater occipital (second and third dorsal nerves)
Auriculotemporal (mandibular nerve)
Zygomaticotemporal, zygomaticofacial (zygomatic [maxillary] nerve)
Supraorbital (ophthalmic nerve)
Supratrochlear (ophthalmic nerve)
Technique
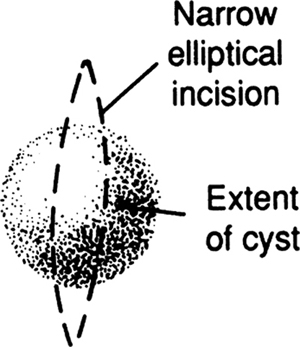
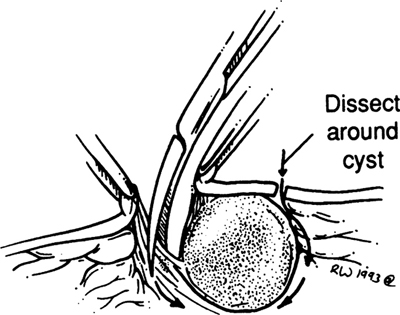
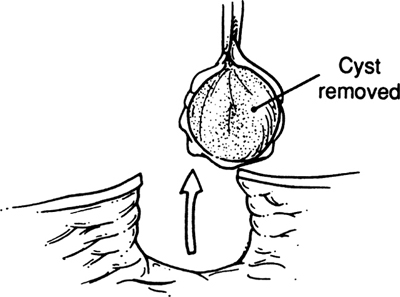
Benign Skin Lesions (Figs. )
Benign skin lesions fall into several groups. Cystic lesions include epidermal inclusion cysts, sebaceous cysts, pilonidal cysts, and ganglia. Another group includes warts, keratoses, keloids, hemangiomatas, arteriovenous malformations, glomus tumors, and capillary malformations.
A third group includes decubitus ulcers, hidradenitis suppurativae, and burns. Junctional, compound, and intradermal nevi and malignant lentigos compose another group.
Step 1.
For a cyst, make an elliptical incision. For a noncystic lesion, be sure to include approximately 0.5 cm of tissue beyond the lesion when making the elliptical incision.