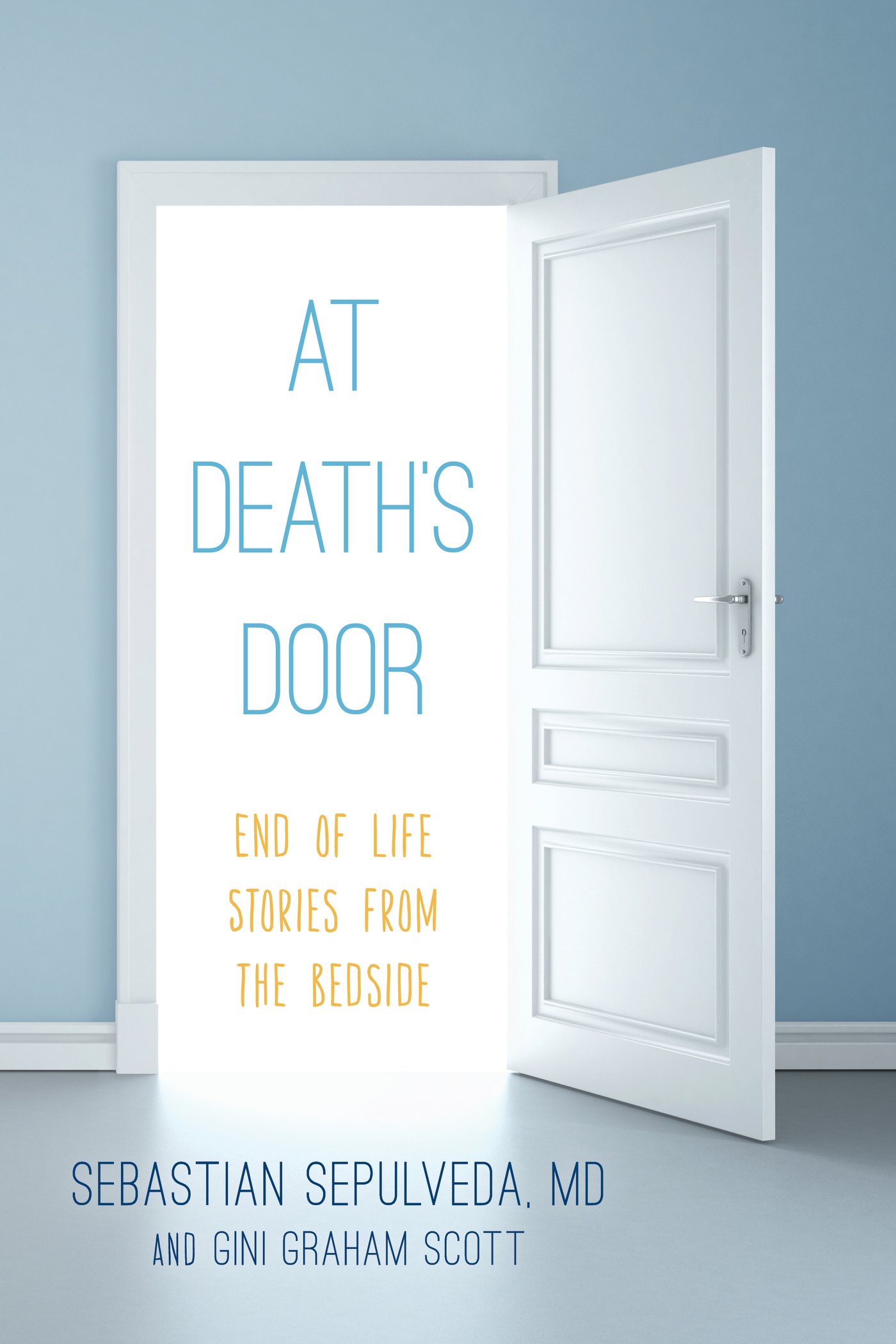
At Death's Door
At Death's Door
End of Life Stories from the Bedside
Sebastian Sepulveda
and Gini Graham Scott
ROWMAN & LITTLEFIELD
Lanham Boulder New York London
Published by Rowman & Littlefield
A wholly owned subsidiary of The Rowman & Littlefield Publishing Group, Inc.
4501 Forbes Boulevard, Suite 200, Lanham, Maryland 20706
www.rowman.com
Unit A, Whitacre Mews, 26-34 Stannary Street, London SE11 4AB
Copyright 2017 Sebastian Sepulveda
This book is not intended as a medical manual, and the data presented here are meant to assist the reader in making informed choices regarding wellness. This book is not a replacement for treatment(s) that the reader's personal physician may have suggested. If the reader believes he or she is experiencing a medical issue, professional medical help is recommended. Mention of particular products, companies, or authorities in this book does not entail endorsement by the publisher or author.
All rights reserved. No part of this book may be reproduced in any form or by any electronic or mechanical means, including information storage and retrieval systems, without written permission from the publisher, except by a reviewer who may quote passages in a review.
British Library Cataloguing in Publication Information Available
Library of Congress Cataloging-in-Publication Data
Names: Sepulveda, Sebastian, 1960- author.
Title: At death's door : End of life stories from the bedside / Sebastian Sepulveda and Gini Graham Scott.
Description: Lanham : Rowman & Littlefield, 2017. | Includes bibliographical references and index.
Identifiers: LCCN 2016032742 (print) | LCCN 2016034056 (ebook) | ISBN 9781442273344 (cloth : alkaline paper) | ISBN 9781442273351 (electronic)
Subjects: LCSH: Right to die--Popular works. | Terminal Care--Popular works. | Medical ethics--Popular works. | Death--Planning--Popular works.
Classification: LCC R726 .S448 2017 (print) | LCC R726 (ebook) | DDC 362.17/5--dc23
LC record available at https://lccn.loc.gov/2016032742
 TM The paper used in this publication meets the minimum requirements of American National Standard for Information Sciences Permanence of Paper for Printed Library Materials, ANSI/NISO Z39.48-1992.
TM The paper used in this publication meets the minimum requirements of American National Standard for Information Sciences Permanence of Paper for Printed Library Materials, ANSI/NISO Z39.48-1992.
Printed in the United States of America
Introduction
As a doctor specializing in hospital inpatients and in my own private practice, I have encountered many patients and families who approach death in very different ways. Their attitude and decision as to whether or not to choose a DNR (do not resuscitate) or DNI (do not intubate) order affects the kind of treatment they get at the end. Another factor that influences their treatment is the view of family members when patients can no longer make these end-of-life treatment decisions, such as if a patient has slipped into a coma or has a serious stroke or other mental disability so he or she cant think logically or even talk. Then, someone else has to decide. In some cases, patients have given clear instructions to their doctor and family on what to do at the end; but often they dont, which can make determining what to do difficult.
As the doctor who has cared for these patients in their final days, I can only provide advice on what to do, if they can understand, or advise their family and sometimes their personal physician if the patients cant understand themselves. However, I often find that their physician has withdrawn and turned their end-of-life care to the hospital. So I often have to sort out these decisions with the patient, family, or sometimes both, where the family still consults with the patient.
Whatever the case, being a doctor at the end of a patients life has its special challenges, especially today because the advances of modern medicine make it technologically possible to do much more to prolong a patients life. But complicating the situation is the concern of both the patient and family about the difficulties at the end of life, most notably the increasing deterioration of the body and mind, along with the increasing pain.
While a doctors long-standing ethical commitment is to provide the best possible care and maintain life, this commitment is challenged by changing attitudes about whether to alleviate pain as possible or provide medication that may end the patients suffering by ending life. In almost all states today except for five of them, providing any treatment to end the patients life is still illegal. However, the notion of assisted suicide in the face of a terminal illness seems to be growing in acceptance, as reflected in the case of Brittany Maynard. She went to Oregon, which permits such suicides under its Death with Dignity Law, and on November 1, 2014, she took a lethal dose of drugs prescribed by her doctor to end her suffering. She stated that death with dignity was the best option for me and my family.
Yet despite these changing laws and public attitudes, as a doctor I am still committed to preserving life as long as possible, while relieving suffering. In that spirit I have approached end-of-life care to work with each patient as long as I can, as well as with any family members who are present at the end.
At Deaths Door has been written from this perspective to provide an inside look at how a doctor deals with dying patients and their families. As it illustrates, every patient is different, because they vary so greatly in the condition that has led them to this end-of-life dying process, in the support they receive from family members and friends, and in their own attitude toward what is happeningranging from anger and denial to acceptance and even humor. While some patients feel the love around them, which helps them feel better physically, emotionally, mentally, and spiritually, others experience dying alone, which may contribute to their resistance and denial. I even had one patient who, though morbidly obese and without any family or friends to visit, found the humor in his situation and made jokes about what he was experiencing. Perhaps this humor was his way to distance himself from an otherwise painful and hard-to-accept reality. Eventually, toward the end, he finally accepted the truth of his condition and two days later, he died.
Catherine E. Shoichet, Brittany Maynard, Advocate for Death with Dignity Dies, CNN.com, November 3, 2014, http://www.cnn.com/2014/11/02/health/oregon-brittany-maynard.
The California End of Life Option Act and Death with Dignity, Death with Dignity, January 22, 2016, https://www.deathwithdignity.org/news/2016/01/california-end-of-life-option-act; Sounmya Karlamangla, How Californias Aid-in-Dying Law Will Work, Los Angeles Times, May 12, 2016.
Chapter 1
Caring for End-of-Life Patients
In writing this work, I have described my everyday experiences in dealing with patients in their last days of life, and with family members, relatives, and medical professionals involved in their care. At times, these interactions have included religious leaders, such as ministers, priests, and rabbis, who provided guidance and support for some patients in their last difficult days.
To fully understand what happens in caring for patients, it is also important to understand the hospital system and the other organizations and companies providing end-of-life care and services. Now that individuals are living longer and healthier lives, end-of-life care has gotten increasing attention, and a growing new profession of doctors and other medical care providers has emerged to deal with these patients. I am one of the thousands of such professionals, although the newness of this profession means that the vast majority of people in the United States havent heard of us.
Next page




 TM The paper used in this publication meets the minimum requirements of American National Standard for Information Sciences Permanence of Paper for Printed Library Materials, ANSI/NISO Z39.48-1992.
TM The paper used in this publication meets the minimum requirements of American National Standard for Information Sciences Permanence of Paper for Printed Library Materials, ANSI/NISO Z39.48-1992.