Ole T. Jensen - The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone Reconstruction
Here you can read online Ole T. Jensen - The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone Reconstruction full text of the book (entire story) in english for free. Download pdf and epub, get meaning, cover and reviews about this ebook. year: 2009, publisher: Quintessence Pub Co, genre: Home and family. Description of the work, (preface) as well as reviews are available. Best literature library LitArk.com created for fans of good reading and offers a wide selection of genres:
Romance novel
Science fiction
Adventure
Detective
Science
History
Home and family
Prose
Art
Politics
Computer
Non-fiction
Religion
Business
Children
Humor
Choose a favorite category and find really read worthwhile books. Enjoy immersion in the world of imagination, feel the emotions of the characters or learn something new for yourself, make an fascinating discovery.
- Book:The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone Reconstruction
- Author:
- Publisher:Quintessence Pub Co
- Genre:
- Year:2009
- Rating:3 / 5
- Favourites:Add to favourites
- Your mark:
The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone Reconstruction: summary, description and annotation
We offer to read an annotation, description, summary or preface (depends on what the author of the book "The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone Reconstruction" wrote himself). If you haven't found the necessary information about the book — write in the comments, we will try to find it.
Contents
Section I: Biologic Rationale
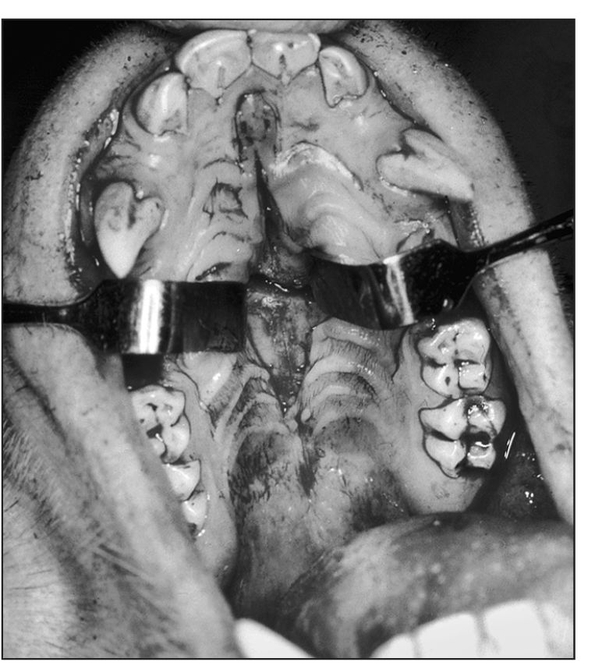
1. Biologic Basis of the Osteoperiosteal Flap
2. A New Biologic Classification of Bone Augmentation
Section II: Distraction Osteogenesis Techniques
3. Alveolar Distraction Osteogenesis
4. Supraperiosteal Transport Distraction Osteogenesis
5. Rapid Alveolar Expansion of Osteoperiosteal Flaps
Section III: Pedicled Segmental Osteotomy Techniques
6. Book Bone Flap
7. Island Osteoperiosteal Flap
8. Internal Alveolar Split Bone Graft
9. Sandwich Osteotomy Bone Graft in the Anterior Maxilla
10. Sandwich Osteotomy Combined with Extraction Socket Bone Graft
11. Sandwich Osteotomy Bone Graft in the Anterior Mandible
12. Smile Osteotomy
13. Sinus Graft Combined with Osteoperiosteal Flaps
14. Maxillary Alveolar Split Horseshoe Osteotomy
15. Sinus Floor Intrusion as a Vascularized Osteoperiosteal Flap
Section IV: Restorative Techniques
16. Alveolar Design by Stereolithography
17. Esthetically Driven Prosthetic Management of Osteoperiosteal Flaps
18. Esthetically Driven Surgical and Prosthetic Management of Alveolar Distraction Osteogenesis
19. Recombinant Protein Application for Bony and Periodontal Augmentation
20. Dental Implant Repositioning by Osteotomy in the Esthetic Zone
Section V: Developing Technologies
21. Osteoperiosteal Tissue-Engineered Injectable Bone
22. De Novo Tooth Engineering to Replace Lost Teeth
Ole T. Jensen: author's other books
Who wrote The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone Reconstruction? Find out the surname, the name of the author of the book and a list of all author's works by series.


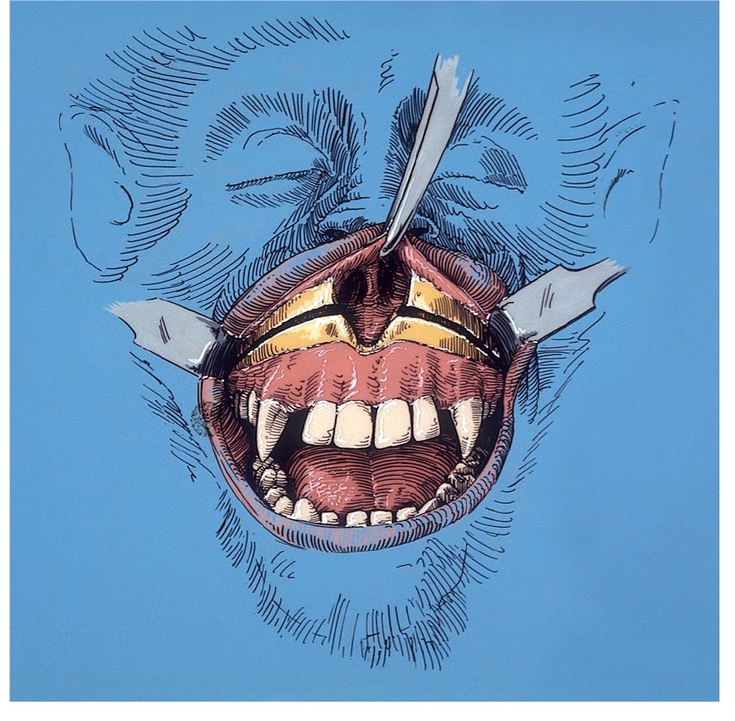

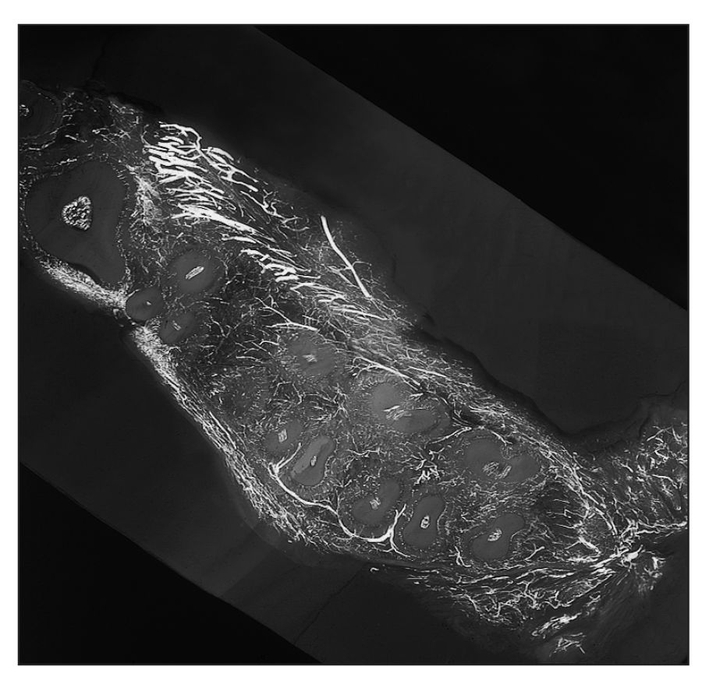
 Biology of Wound Healing
Biology of Wound Healing