Copyright 2019 by Nicole Redvers. All rights reserved. No portion of this book, except for brief review, may be reproduced, stored in a retrieval system, or transmitted in any form or by any meanselectronic, mechanical, photocopying, recording, or otherwisewithout the written permission of the publisher. For information contact North Atlantic Books.
Published by
North Atlantic Books
Berkeley, California
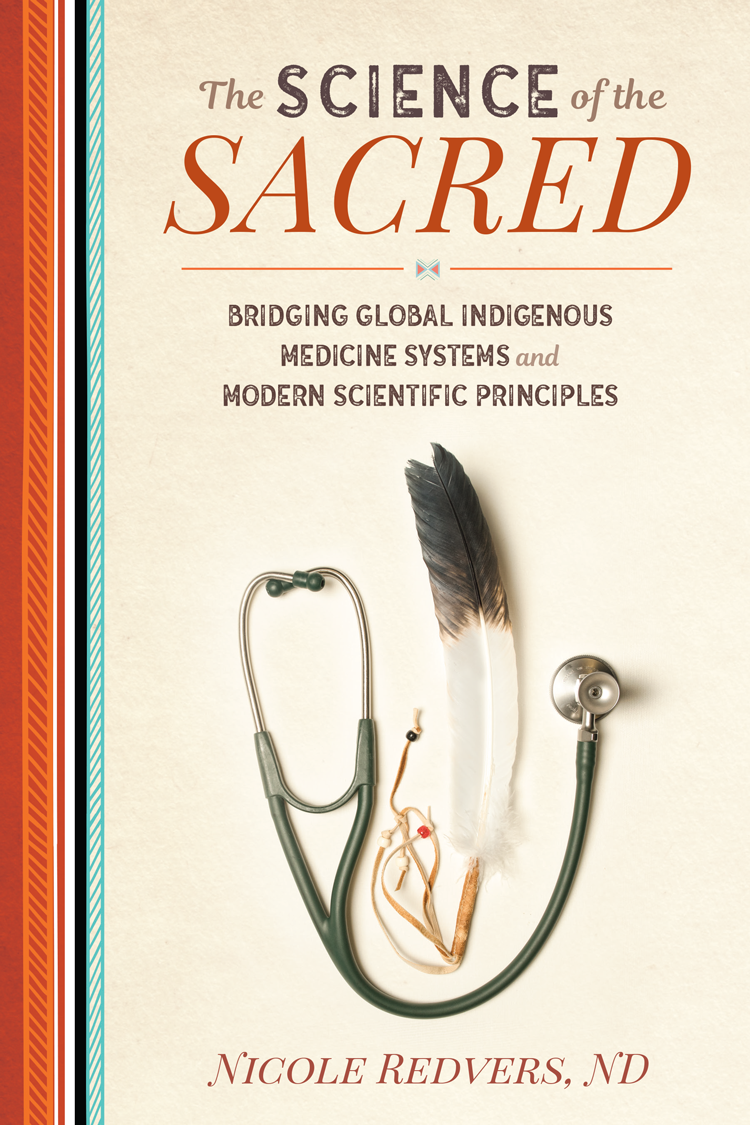
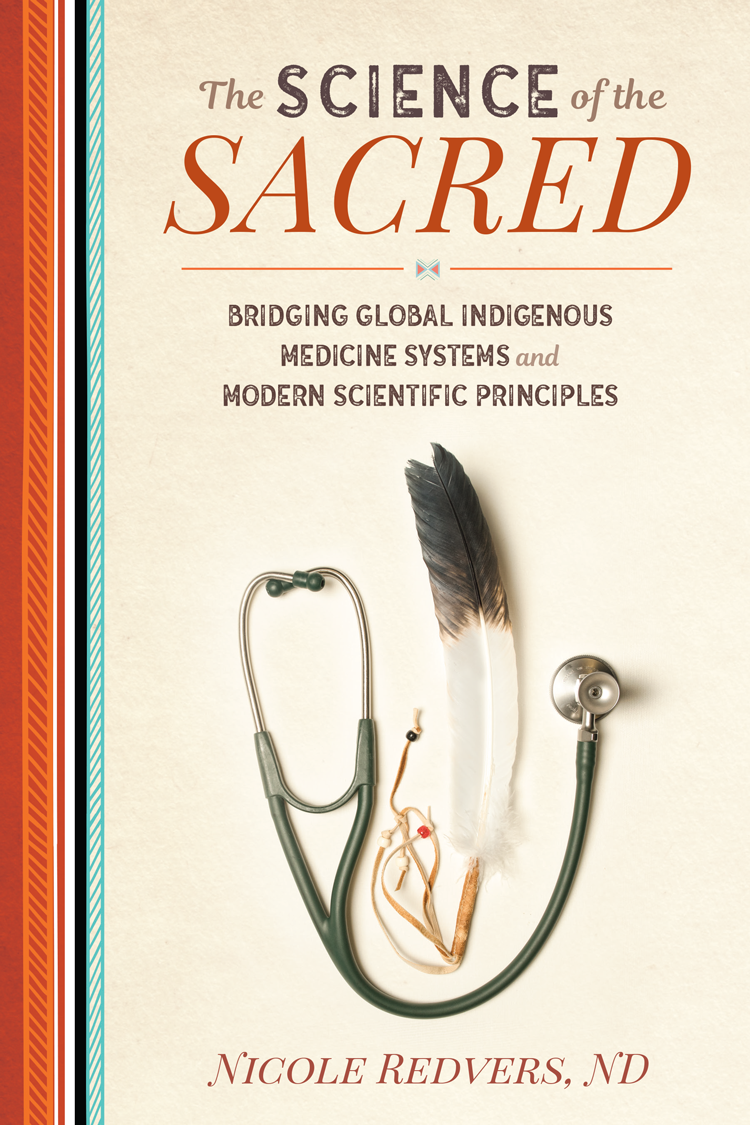
Cover photo by Dave Brosha
Cover design by Jasmine Hromjak
Book design by Happenstance Type-O-Rama
Author photograph by Angela Gzowski
Printed in the United States of America
The Science of the Sacred: Bridging Global Indigenous Medicine Systems and Modern Scientific Principles is sponsored and published by the Society for the Study of Native Arts and Sciences (dba North Atlantic Books), an educational nonprofit based in Berkeley, California, that collaborates with partners to develop cross-cultural perspectives, nurture holistic views of art, science, the humanities, and healing, and seed personal and global transformation by publishing work on the relationship of body, spirit, and nature.
North Atlantic Books publications are available through most bookstores. For further information, visit our website at www.northatlanticbooks.com or call 800-733-3000.
Library of Congress Cataloging-in-Publication Data
Names: Redvers, Nicole, author.
Title: The science of the sacred : bridging global indigenous medicine
systems and modern scientific principles / Dr. Nicole Redvers.
Description: Berkeley, California : North Atlantic Books, [2019].
Identifiers: LCCN 2018038359 (print) | LCCN 2018039072 (ebook) | ISBN
9781623173371 (e-book) | ISBN 9781623173364 (paperback)
Subjects: | MESH: Medicine, Traditional | Science | Health Knowledge,
Attitudes, Practice | Philosophy, Medical
Classification: LCC R733 (ebook) | LCC R733 (print) | NLM WB 55 | DDC
610dc23
LC record available at https://lccn.loc.gov/2018038359
North Atlantic Books is committed to the protection of our environment. We partner with FSC-certified printers using soy-based inks and print on recycled paper whenever possible.
The author gratefully acknowledges the financial support of the NWT Arts Council/GNWT for the production of this book.

Every reasonable effort has been made to trace ownership of copyright materials. Information enabling the publishers to rectify any reference or credit in future printings will be welcomed.
The information in this book is not intended as a substitute for medical or professional advice. It is strictly the opinion of the author. It is recommended that you consult your professional healthcare provider if you have any physical, mental, or emotional health concerns.
To all the Elders, the most brilliant scientists of them all
For wise men, nothing that exists
Remains unseen; they do not share
The idle dreams of would-be scholars.
Only the artist, not the fool
Discovers that which nature hides.
Introduction
H uman beings are arguably among the most complex creatures on this planet (at least we like to think so). With our highly developed social structures and lifestyles, you would think we could have most things figured out. Yet somehow in the development of our complexity, we have forgotten about the simple things that make us well. We continue to get sicker and sicker, with no end in sight. The promise of new medical discoveries for various cures, and the abolishment of certain diseases, always seem to be just on the horizon and never closer.
As Albert Einstein stated and has often been quoted, The definition of insanity is doing the same thing over and over again and expecting different results. In this regard, the healthcare delivery patterns in developed countries have essentially been the same for the last century. New treatments, tests, and scientific advances have occurred; however, the fundamental basis of day-to-day medical practice has remained stagnant: patient in, prescription written, patient out.
As we continue to update our practices and applications, we mold medical care on the same delivery model and expect different results. Not only that, we apply and hold up the Western biomedical model to all populations under the Health Governance Structure. Regardless of ethnicity, belief system, and cost, primary-care delivery remains the same at its base, with outskirt satellite operations occasionally providing care in culturally specific ways. We base most decisions on evidence-based practice instead of including evidence-informed practice, which is an important clarification that needs to be understood.
The evidence is telling us, however, that the times are changing in regard to what the general populace desires from their healthcare experience. Individuals and families are becoming increasingly unsatisfied with the patient-in, prescription-written, patient-out model of communication and delivery encapsulated in a five- to fifteen-minute person-to-person interaction. As a result, we see definite examples of practitioners and jurisdictions that are open minded enough to listen to those desires. Riding the wave of change are institutions such as the Cleveland Clinic Center for Functional Medicine; Anishnawbe Health Toronto (AHT); the Cancer Treatment Centers of America (CTCA); the University of Arizona Integrative Health Center (UAIHC); the Hospital of Integrated Medicine in Pitigliano, Italy; Scarborough Hospitals Centre for Integrative Medicine (CIM) in Toronto; and regulated naturopathic medical programs in North America recognized by the Council on Naturopathic Medical Education (CNME).
We also see examples of practitioners and institutions that seem to resist any change to the status quo. This could be for various reasons that can be substantiated by the lens through which they view medical care, debatably however, at risk of remaining frozen in medical bureaucracy (and cost). This status quo then often assumes, often unknowingly, an antagonistic attitude toward people who desire freedom of choice in their healthcare delivery (this point has been brought to light more recently with the passing of Section 2706 of the US Affordable Care Act, which is titled Nondiscrimination in Health Care). As the years go on and the structure of medicine remains solid in its convictions (and costliness), more patients will turn to more personalized care to deal with the broader range of chronic disease symptoms and diagnoses that will continue to dominate our human state for the foreseeable future.
Most people on the planet pay for their healthcare. Even individuals in countries such as Canada, which offer free healthcare, pay for it every day with their taxes through their purchases and employment, or in premiums to insurance companies for drug and benefit plans. We must forget this illusion of free healthcare, as it never has truly existed and never will exist in the conventional sense. What differs is our ability to access care based on how we pay into our healthcare institutions. The research organization IQVIA Institute predicts that global spending on prescription medicines will reach nearly $1.5 trillion by 2021, up nearly $370 billion from 2016 spending. If public healthcare systems continue to be completely and utterly reliant on private profit-making corporations, we will have a hard time trying to explain away our free medical systems as we lose access to more and more unaffordable medications.
Next page