Contents
Guide
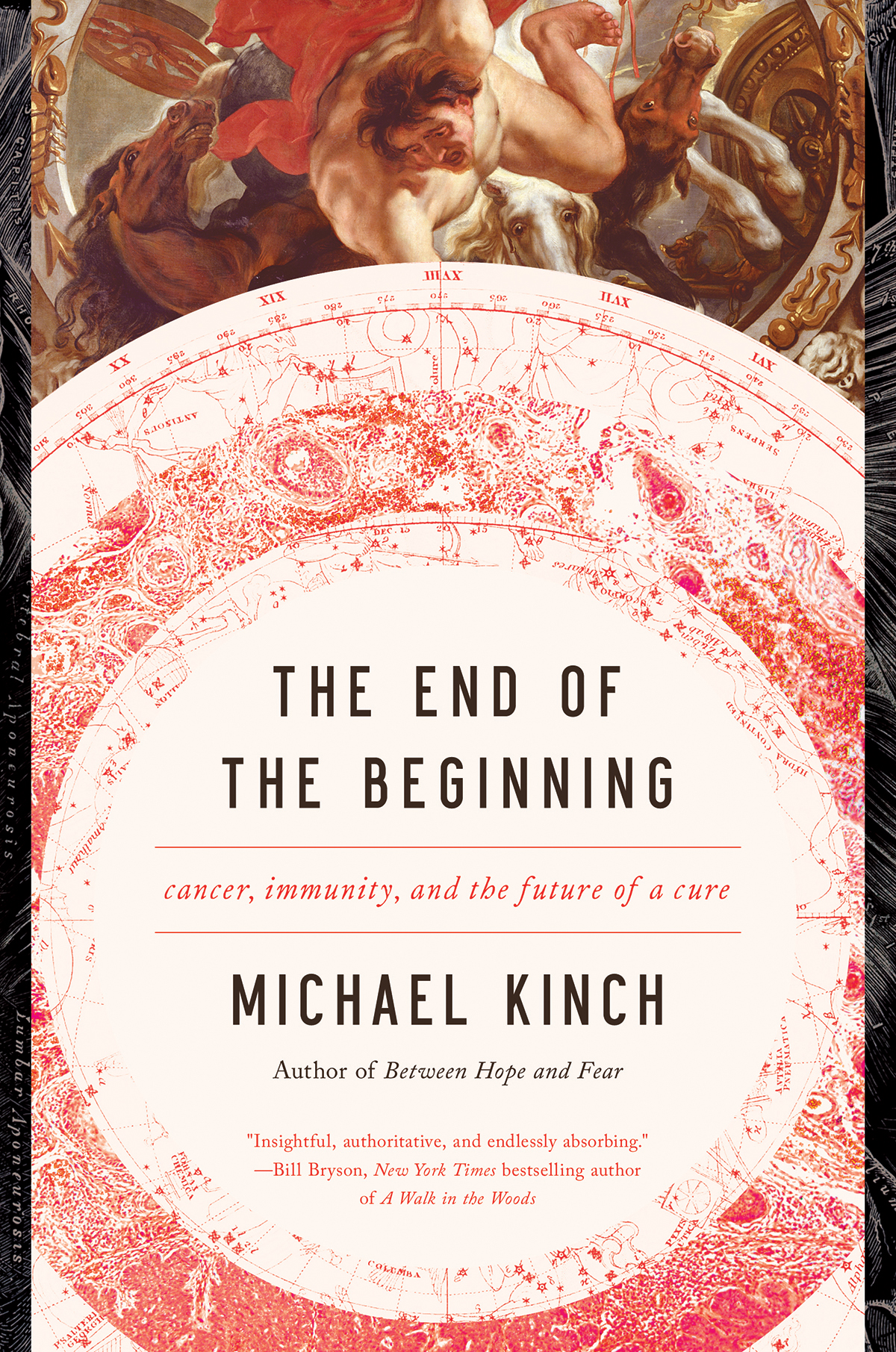
THE END OF
THE BEGINNING
Cancer, Immunity, and the
Future of a Cure
MICHAEL S. KINCH
THE END OF THE BEGINNING
Pegasus Books Ltd.
148 W. 37th Street, 13th Floor
New York, NY 10018
Copyright 2019 Michael S. Kinch
First Pegasus Books edition April 2019
Interior design by Maria Fernandez
All rights reserved. No part of this book may be reproduced in whole or in part without written permission from the publisher, except by reviewers who may quote brief excerpts in connection with a review in a newspaper, magazine, or electronic publication; nor may any part of this book be reproduced, stored in a retrieval system, or transmitted in any form or by any means electronic, mechanical, photocopying, recording, or other, without written permission from the publisher.
Library of Congress Cataloging-in-Publication Data is available.
ISBN: 978-1-64313-025-5
ISBN: 978-1-64313-108-5 (ebk.)
Distributed by W. W. Norton & Company, Inc.
www.pegasusbooks.us
This book is dedicated to the memories and families of Harold Noe, Thomas Noe, William Zellner, and all the victims of cancer hoping the beginning of the end is near
CONTENTS
I t was the same campus, the same sunny day, and almost the exact same parking spot I had occupied just a few weeks before. However, the circumstances could not have been more different. On my previous trip, I was an invited guest, hosted by a former colleague to present the highlights from the cutting-edge oncology research we were conducting at a biotechnology company just a few miles up the road from the National Institutes of Health (NIH) Bethesda, Maryland, campus where I was currently standing. The name of the company was MedImmune, a conflation of two words meant to reflect a focus on developing novel ways of unleashing the power of the immune system to promote medicine. While the company had already made a name for itself in infectious diseases, I had been tasked with building a portfolio of products to target cancer. The company was largely focusing its efforts to unharness the power of monoclonal antibodies, the guided missiles of the immune system that can be as specific and destructive as the most advanced smart bombs that were used in the second Gulf War just two years before.
I had been recruited from Purdue University, where my academic work as a professor had led to the discovery of ways monoclonal antibodies could be created and deployed to seek out and destroy metastatic cells. These rogue killers comprise the most invasive and deadly tumor cells and tend to elude both the surgeons knife and chemotherapy. My tenure at Purdue had been granted just a year or two earlier and I was happily obsessed with understanding the processes behind metastasis. Nonetheless, throughout these halcyon academic years, I had always been gripped with a passion to apply research to alleviate human suffering in the real world, which was quite distinct from trying to cure experimental mouse tumors, the mainstay of academic research.
Nineteen ninety-eight was a pivotal year, though this was not clear to me at the time. I was in my third year as an assistant professor at Purdue and had published a scientific manuscript detailing a project initiated while transitioning from my postdoctoral studies at the Lineberger Cancer Center at the University of North Carolina to my start at Purdue. We had identified a type of cellular behavior distinguishing benign cells from their malignant counterparts and I hoped these differences might provide a new opportunity for targeting cancer.
I have been extraordinarily lucky to be in the right place and time at key points. Working in 1995 with colleagues at Chapel Hill and at nearby Glaxo Pharmaceuticals (located down the road in Research Triangle Park, North Carolina), we innovated a novel approach to create monoclonal antibodies to characterize or, if we were very lucky, actually convey some use in targeting metastatic cancer. Our rationale back in 1995 was based upon emerging evidence for a new approach using monoclonal antibodies as a much-needed alternative to conventional chemical toxins. Only one monoclonal antibody had ever been approved for cancer at the time.
The drug Rituxan (rituximab), as we will see, had been developed by a start-up biotechnology company in San Diego (IDEC Pharmaceuticals) and marketed by another biotechnology company located outside San Francisco (Genentech). Rituximab had overcome all the hurdles necessary to be approved by the Food and Drug Administration (FDA) in 1997 and it was to be used in the battle against a type of blood cancer known as a lymphoma . Early sales of the drug were promising but not overwhelming. The reason for the lag in sales was in part because monoclonal antibody drugs were not very familiar to most physicians (or even many scientists). However, this drug would go on to log peak annual revenues of more than $7.3 billion in 2015 alone and become the twelfth-highest selling drug in history (undoubtedly fated to move even higher because antibody drug sales are not as susceptible to generic competition as more conventional medicines are).
Looking back to 1998, the commercial view of monoclonal antibody therapeutics was not terribly optimistic. For one thing, the nascent field was considered, by many industry experts, to be unrealistic based on economics alone. Such views were justified based on the high costs needed to manufacture these large molecules, which might cost hundreds of dollars per dose (as compared with pennies for many conventional medicines). Moreover, key patents filed by early biotechnology pioneers meant a substantial portion of revenuesas much as one-third for some medicineswould have to be surrendered to competitors. To break even, some antibody drug companies contemplated asking prices of up to $10,000 for a single course of treatmentan outrageous proposition at the time.
Ten thousand dollars today seems almost like a bargain, when insurance companies are, with increasing frequency, asked to spend hundreds of thousands or even millions of dollars on some medicines. However, this price tag seemed utterly absurd to many in the late 1990s. Hence, many conventional pharmaceutical companies focused on standard medicines comprised of small and less complex molecules (think of aspirin). In contrast, monoclonal antibodies were large and unwieldy beasts (e.g., a thousand times larger than aspirin). To manufacture a single antibody requires the precise arrangement of four large proteins, each situated in just the right way, to ensure an antibody drug is stable, safe, and efficacious.
This complex construction could not be performed in the massive fermentation tanks used to manufacture small molecules but instead required something with far greater sophistication: the honed skills of human or other mammalian cells. Yes, these cells actually served as the factories, and the technology needed to engineer the production of proteins in these tiny workshops had only been enabled in the 1970s and 1980s. All the antibody drugs described herein were produced by cells obtained from discarded human or animal tissues and then modified using genetic engineering to produce the antibody of interest.
The high costs of growing the antibody-producing cells, purifying their protein products, and ensuring the resultant drug remained viable accounted for for the bulk of the expense of monoclonal antibody drugs. These costs were compounded by an enormous amount of intellectual property (patents and royalties) that drastically increased the cost of manufacturing antibodies. Consequently, there were few biotechnology companies, or more accurately, investors, willing to take the plunge into such a risky enterprise. In my years as an academic, I spoke with representatives from many conventional pharmaceutical companies and most indicated their unease with utilizing monoclonal antibodies for any indication, and certainly not for cancer.