Part 1
Neurophysiology
Laurent Misery and Sonja Stnder (eds.) Pruritus 10.1007/978-1-84882-322-8_1 Springer-Verlag London Limited 2010
1. Neuroanatomy of Itch
Akihiko Ikoma 1
(1)
Department of Dermatology, University of California, San Francisco, San Francisco, USA
Abstract
Peripheral tissues that can produce an itching sensation are the skin, the conjunctiva and the mucous membrane. In the skin, sensory nerves innervate the epidermis as well as the dermis and the subcutaneous fat tissue, although the autonomic nerves never innervate the epidermis. However, the sensory nerves causing the itching sensation seem to be located in a restricted part of the skin. Histamine has been known for decades to be a potent pruritogen in human beings and, for example, plays a key role in urticaria-associated pruritus.1 The sensation induced by experimentally applied histamine is, however, not always itchy. Itch is a sensation mainly induced when histamine is applied to the skin by iontophoresis or by pricking, while it is rather painful when subcutaneously injected.2 Clinically, release of histamine from mast cells in the upper dermis leads to urticaria that is characterized by wheal, flare and itching sensation. On the other hand, histamine release in the deep dermis or subcutaneous tissue results in angioedema that often associates with pain rather than with itch.3 The sensation caused by skin-burn also depends on the depth of damage. Itch frequently occurs in such damage in a limited and superficial manner or at the last recovering stage, while almost only pain occurs when there is deeper damage. According to a report published half a century ago, a single spicule taken from cowhage (macuna pruriens) pods induced itch most intensely if inserted to the depth of the basal membrane, while itch was never induced if the epidermis and upper dermis had been removed.4 Thus, it has been suggested that the peripheral origin of itch is limited to a superficial layer of skin, especially epidermis and upper dermis around the basal membrane.
1.1 Nerves in the Skin
Peripheral tissues that can produce an itching sensation are the skin, the conjunctiva and the mucous membrane. In the skin, sensory nerves innervate the epidermis as well as the dermis and the subcutaneous fat tissue, although the autonomic nerves never innervate the epidermis. However, the sensory nerves causing the itching sensation seem to be located in a restricted part of the skin. Histamine has been known for decades to be a potent pruritogen in human beings and, for example, plays a key role in urticaria-associated pruritus. Thus, it has been suggested that the peripheral origin of itch is limited to a superficial layer of skin, especially epidermis and upper dermis around the basal membrane.
However, this does not mean that origin of pain is limited to a deeper level. Immunohistochemical ultrastructural investigations have revealed that free nerve endings exist in healthy human epidermis. that associates with pain sensitization in the genital area. This indicates that elongated nerve endings in the epidermis are involved in intensifying sensation even if it is itch or pain, although one cannot still tell whether elongated nerve endings belong to itch or pain nerves since specific receptors to distinguish itch and pain nerves are not yet identified.
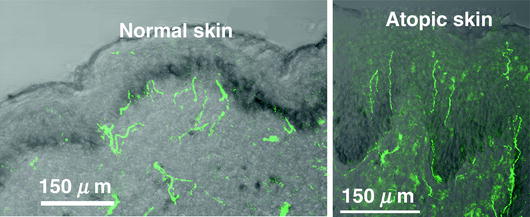
Fig. 1.1
Elongation of free nerve endings into the epidermis in atopic dermatitis. A larger amount of protein gene product 9.5 (PGP9.5) positive nerves are found in the epidermis of atopic dermatitis (Fig. a)
(Courtesy of Prof. Kenji Takamori, Juntendo University, Japan.)
1.2 Primary Afferent Nerves for Itch
Sensory nerves that have nerve endings in the skin can be categorized into three groups: A, A and C nerves (Table
Table 1.1
Classification of primary sensory nerves
| Diameter (m) | Conduction velocity (m/s) | Sensation |
|---|
A | 6-12 | 33-75 | Touch, pressure |
A | 1-5 | 3-30 | Stabbing pain, thermal sense |
C | 0.2-1.5 | 0.5-2 | Burning pain, itch, thermal sense |
Decisive evidence supporting the specific theory has been provided by identification of nerves for histamine-induced itch. Several human microneurography studies in the past had only revealed a weak histamine-induced activation of polymodal C nerves, which failed to explain intense itch. Moreover, the size of their cutaneous receptive field was too small to account for histamine-induced large flare. On the other hand, histamine-sensitive neurons found out among mecha-no-insensitive C nerves (CMi) were activated in parallel to the time course of histamine-induced itch and their receptive field size of CMi nerves was larger than that of polymodal C nerves and therefore consistent with a large flare size.
Table 1.2
Differences between histamine-sensitive and polymodal C nerves
| Histamine-sensitive C nerves | Polymodal C nerves |
|---|
Sensation | Itch | Pain |
Percentage | | |
Sensitivity to mechanical stimuli | No | Yes |
Innervating skin area | Large | Small |
Conduction velocity | 0.5 m/s | 0.5-2 m/s |
Threshold to electrical stimuli | High | Low |
Spontaneous activity | No | Yes |
Though identification of primary afferents for histamine-induced itch was a breakthrough in itch research, histamine-responsive CMi nerves are not able to explain other types of itch. While histamine-induced itch always accompanies axon-reflex flare, itch without flare is experienced in our daily life. Itch induced by insertion of cowhage spicules to the skin does not accompany any axon-reflex flare. A study, recently reported, supports that cowhage-induced itch appears to be mediated by a subpopulation of capsaicin-sensitive afferent nerves that can be separated from those conducting histamine-induced itch. Thus, there seems to be more than one peripheral neural pathway for itch.
1.3 Secondary Afferent Nerves for Itch
The neurons of primary afferent nerves for skin-originating pain are located in the dorsal root ganglions (DRG) and are relatively small among DRG neurons, this also supports the presence of itch-specific transmission mechanism at the spinal level.
Fig. 1.2
Neural pathway for histamine-induced itch. H1R, histamine H1 receptor; CMi, mechano-insensitive C nerve; DRG, dorsal root ganglion; STT, spinothalamic tract