Giuseppe Micali , Marco Cusini , Pompeo Donofrio and Franco Dinotta Atlas of Male Genital Disorders A Useful Aid for Clinical Diagnosis 10.1007/978-88-470-2787-9_1 Springer-Verlag Italia 2013
1. Anatomy of Male Genitalia
Franco Dinotta 1 , Maria Rita Nasca and Guiseppe Micali
(1)
Center for Sexually Transmitted Diseases Dermatology Unit Dipartimento di Specialit Medico-Chirurgiche, AOU Policlinico Vittorio Emanuele Presidio G. Rodolico, Catania, Italy
Abstract
Male genitalia include the penis and scrotum.
Anatomy
Male genitalia include the penis and scrotum.
The penis is formed by two dorsal erectile structures ( corpora cavernosa ) and one ventral midline body ( corpus spongiosum ) which contains the urethra. These structures, covered by a thin and glabrous skin containing both apocrine and eccrine sweat glands, form the shaft of the penis. The corpus spongiosum is distally enlarged and rounded to form the glans, covered by semimucosa and topped by a vertical slit corresponding to the external urethral meatus . The base of the glans is called corona and it is proximally delimited by the coronal sulcus in which the secretion of freestanding balanopreputial sebaceous glands ( Tyson glands ) and epithelial debris, called smegma , may collect. The glans shows ventrally a linear cord, called frenulum , which extends from the urethral meatus to the coronal sulcus. When the frenulum is too short, erection may be painful and frenulotomy may be required. In uncircumcised men the glans is covered by a skin fold, called prepuce or foreskin . The foreskin is separated from the glans by a fold called preputial sac . The inner foreskin (semimucosa) is separated from the outer foreskin (skin) by a virtual boundary, the preputial ring , which may be narrowed as a result of inflammatory genital disorders, causing phimosis. A longitudinal line, corresponding to the area of conjunction during embryonal development ( median raphe ), is evident on the skin of the midventral shaft. The median raphe may be clearly raised or hyperpigmented in some subjects.
The scrotum is a sac, located below the shaft and between the inguinal folds, that contains the testicles that are attached to the deferent ducts. It is medially divided into two virtual cavities separated by an internal septum that corresponds, on the scrotal surface, to a skin groove called the scrotal raphe . The skin of the scrotum is usually thin and elastic and, in adults, it is pigmented and covered by hairs. It also contains both sweat (eccrine and apocrine) and sebaceous glands.
Male genitalia, especially the penis, have a rich vascularization and innervation.
Fig. 1.1
Dorsal appearance of male genitalia. A Penile shaft. B Foreskin. C Coronal sulcus. D Corona. E Glans. F Urethral meatus. G Scrotum
Fig. 1.2
Ventral appearance of male genitalia. A Frenulum. B Foreskin. C Penile median raphe. D Scrotal median raphe. E Inguinal fold
Giuseppe Micali , Marco Cusini , Pompeo Donofrio and Franco Dinotta Atlas of Male Genital Disorders A Useful Aid for Clinical Diagnosis 10.1007/978-88-470-2787-9_2 Springer-Verlag Italia 2013
2. Infections
Marco Cusini 1 , Stefano Ramoni , Salvatore Ferraro and Franco Dinotta
(1)
Center for Sexually Transmitted Diseases Dermatology Unit Dipartimento di Anestesiologia, Terapia Intensiva e Scienze Dermatologiche, Fondazione IRCCS Ca Granda Ospedale Maggiore Policlinico, Milan, Italy
Abstract
Definition : Genital Warts (GW) are viral infections that affect the genital and perigenital area and seldom if ever evolve into cancer.
Genital Warts
Definition : Genital Warts (GW) are viral infections that affect the genital and perigenital area and seldom if ever evolve into cancer.
Etiology : GW are caused by some genotypes of Human Papilloma Virus (HPV), a DNA virus. In most cases infection follows sexual contact and it is a sexually transmitted disease. Low-risk HPV 6 and 11 are common causative agents, with a high efficacy of transmission (about 80%) and, fortunately, poor or no oncogenic potential. High-risk HPV 16 and 18 account for a low transmission percentage.
Epidemiology : genital HPV infection is very common; GW are the most frequent sexually transmitted infection in the Western world. Men and women are equally affected. GW are frequently encountered from age 20 to 45.
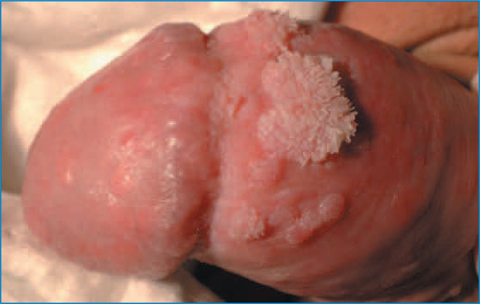
Clinical appearance : GW are clinically characterized by raised papular lesions that may become confluent (condyloma acuminatum). GW may be skin-coloured, pink, or brown, and may occur as verrucous lesions with a typical cauliflower appearance, or as papillomatous lesions (plaque or peduncolated lesions). Giant GW, also called Buschke- Lwenstein tumors, are uncommon. GW frequently develop on the foreskin and at the coronal sulcus and on the shaft and glans, but they may also extend to the urethral meatus and urethra.
Clinical course : after infection, HPV can remain clinically silent or induce the onset of visible lesions that can progress in number and size, remain stable or spontaneously disappear. HPV infection by high risk oncogenic HPVs may cause the development of genital malignancy.
Diagnosis : in the great majority of cases, diagnosis is based exclusively on clinical observation and past medical history. The use of acetic acid to enhance detection of subclinical infection is limited by its low specificity. Histology should be reserved to selected cases, such as immune-suppressed patients. Nuclear Antigen Amplification Technique (NAAT) is of no use in the routine clinical management of GW. Dermatoscopy may be helpful in the evaluation of initial or equivocal lesions; it shows, in papular lesions, a whitish network circumscribing areas centered by dilated glomerular vessels ( mosaic pattern ), and, in cauliflower- like lesions, irregular whitish projections arising from a common base and comprising elongated and dilated vessels ( finger-like pattern ).
Therapy : lesions may spontaneously regress in immunocompetent patients. The aim of therapy is to treat visible lesions and reduce the risk for sexual transmission. Therapeutic tools are usually divided into patient-applied (PA) and health care provider-applied (HCPA) methods. Of the former, imiquimod 5% cream and podophyllotoxin 0.15% cream are suggested in European and American guidelines. Of the HCPA methods, thermocautery, trichloroacetic acid, laser, and surgery are widely used.
Fig. 2.1
Typical papular and papillomatous lesions on the foreskin
Fig. 2.2
Pinkish and flat papules on the shaft ( a ). b Videodermatoscopy (X10) of one lesion shows a whitish network circumscribing areas centered by dilated glomerular vessels (mosaic pattern)