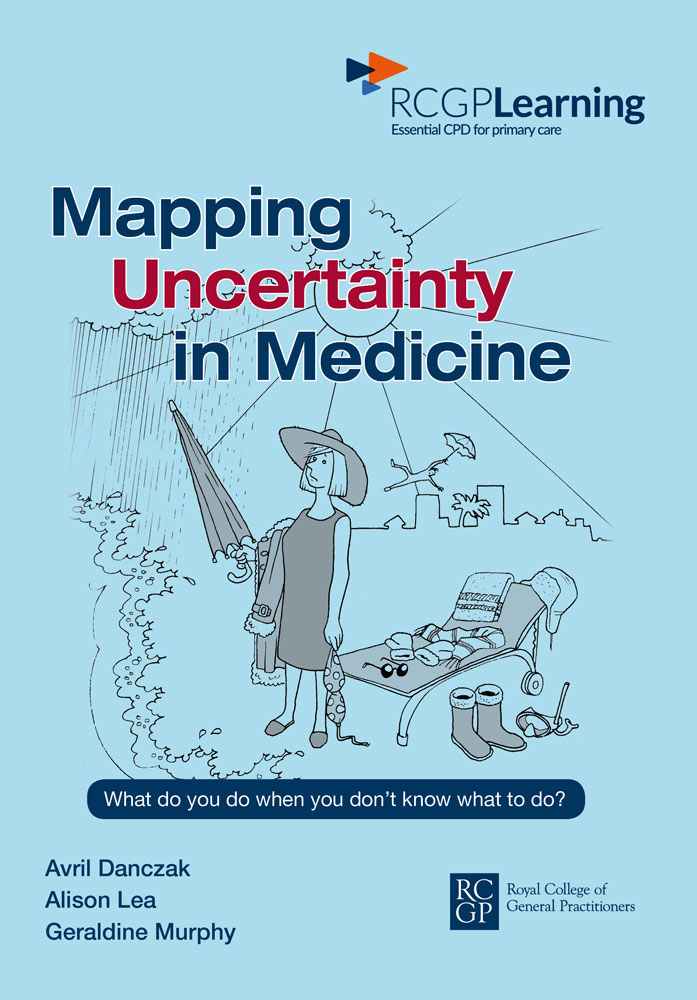
Mapping Uncertainty in Medicine
What do you do when you dont know what to do?
Avril Danczak, Alison Lea and Geraldine Murphy
The Royal College of General Practitioners was founded in 1952 with this object:
To encourage, foster and maintain the highest possible standards in general practice and for that purpose to take or join with others in taking steps consistent with the charitable nature of that object which may assist towards the same.
Among its responsibilities under its Royal Charter the College is entitled to:
Diffuse information on all matters affecting general practice and issue such publications as may assist the object of the College.
British Library Cataloguing-in-Publication Data
A catalogue record for this book is available from the British Library
Royal College of General Practitioners, 2016
Illustrations Andy Howarth, 2016
Published by the Royal College of General Practitioners, 2016
30 Euston Square, London NW1 2FB
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the prior permission of the Royal College of General Practitioners.
Designed and typeset by Prepress Projects Ltd, Perth, UK
Printed by Hobbs the Printer
Indexed by Jim Henderson
ISBN 978-0-85084-416-0
In the varied topography of professional practice, there is a high, hard ground, overlooking a swamp. On the high ground, manageable problems lend themselves to solution through the application of research-based theory and technique. In the swampy lowland, messy, confusing problems defy technical solution. The irony of this situation is that the problems of the high ground tend to be relatively unimportant to individuals or society at large, however great their technical interest may be, while in the swamp lie the problems of greatest human concern. The practitioner must chose. Shall he remain on the high ground where he can solve relatively unimportant problems according to prevailing standards of rigor, or shall he descend to the swamp of important problems and non-rigorous inquiry?
Donald A. Schn
Schn DA. Educating the Reflective Practitioner: toward a new design for teaching and learning in the professions . San Francisco, CA: Jossey-Bass, 1987.
Contents
Every medical student starts his training in a blur of uncertainty but he assumes that the years of training ahead will resolve that blur, as his knowledge and skills become honed in the furnace of medical school and clinical practice. Every Foundation Doctor on her first day braces herself for the unpredictable shift ahead when she is certain to be busy, but assumes she will not know what to do with most of the demands made on her. And every GP starting morning surgery is only certain that by midday he will have been mystified several times (at least!) both by what is wrong with his patients, and by how people cope with the challenges that life throws at them.
Certainty in medicine is an illusion, just as it is in everyday life. A brilliant and experienced surgeon hits a wildly aberrant artery during an operation. A fit young man is rushed into resus from the football field with no cardiac rhythm restored. A baby of normal intrauterine growth pops out from a normal delivery sporting the unforgiving signs of Pierre Robin syndrome. And a woman who you have known as a patient for years bursts into tears and confesses her husband is bullying her, with occasional acts of direct violence. But once we have acknowledged that life is uncertain, and we just have to get on with it, there is still the professional challenge to answer what we can actually do with that uncertainty in clinical practice?
The authors of this book, all practising GPs and educators, have braved this challenge and offer us tools to help us through the labyrinth. They describe a modern paradigm. They take us beyond discussions of sensitivity and specificity or predictive value into the means that we can use to resolve dilemmas discussing with others, using the team, acknowledging the uncertainties with patients, and being disciplined in our own analyses and actions. They encourage conscious acknowledgement and classification of the roots of our uncertainties. They discourage using ways out to resolve our own uncertainty that do not benefit the patient for example, excessive blood tests or referrals. They also encourage physician wellbeing by making uncertainty an issue of conscious competence rather than unconscious stress and anxiety.
Why should you read it? Because it reminds us all that as professionals our job is to reduce uncertainty by systematic history and exam, by diagnostic reasoning, and by conscious labelling of where our uncertainties remain. It is also a very human book reassuring in its acceptance of limits to our knowledge and skills, while challenging us to apply logic to Schns swampy lowland and climb out wherever we can.
If you are uncertain at the end of a consultation, make a note; there will be more you can do to resolve the situation. At the same time, accept it. And keep this book by you it will make sense of your uncertainties.
Prof. Amanda Howe MD MEd FRCGP FAcadMed DCH DRCOG
President-Elect, World Organisation of Family Doctors (WONCA)
Former Vice Chair (Professional Development)
Royal College of General Practitioners
What do you do when you dont know what to do?
While writing this book we have asked this question of many clinicians, from the most junior to the most senior, from academics to jobbing GPs. We always get an immediate response, a wry smile, a grin of relief that told us that every clinician faces this challenge. Those who are most honest will reveal that they face this pretty much every day: sometimes with patients, colleagues, trainees or non-clinical staff, often with families, patients with complex needs or when working on call or out of hours.
Our book is about this, the moment when you dont know what to do, and we refer to this as uncertainty in medicine. As clinicians, all our training, education, continuous professional development, guidelines, protocols and multidisciplinary team meetings are supposed to design out uncertainty and tell us what to do. Strangely, uncertainty doesnt go away with all this effort. Although we know more about medicine than ever, our uncertainty about the way forwards can often seem greater too. In primary care, uncertainty is the norm, as we negotiate the swampy lowlands of daily practice where information is by turns limited, confusing, contradictory, lost, inaccurate and ambiguous. Sometimes we are dealing with complex comorbidities that interact in unknown ways. Sometimes there can seem to be too much information to make sense of. Surrounded by ever increasing scientific knowledge and with limited time, it is hard to decide the best option for the individual patient we are caring for. We hope that this book will help clinicians cope with uncertainty a little more easily.
If you want get straight to work, turn to is likely to help you most.
demonstrates how to use the MUM to understand and manage uncertainty.
explores the psychological aspects of uncertainty, including the reasons why clinicians find it so unpleasant to be uncertain.
covers the teaching and learning of strategies for managing uncertainty and the issues that arise when the uncertainty is about training matters, when it is the educator who does not know what to do.