Introduction to Deep Brain Stimulation: History, Techniques, and Ethical Considerations
Teresa Wojtasiewicz, Nir Lipsman, Jason Gerrard, Travis S. Tierney
Abstract
Deep brain stimulation (DBS) is a procedure that developed as a result of decades of work in stereotactic guidance, neurophysiology, and neuroanatomy. Now, DBS is a validated, Food and Drug Administration (FDA)-approved treatment for a number of neurological and psychiatric disorders including Parkinsons disease, essential tremor, dystonia, obsessive compulsive disorder, and epilepsy. Further applications remain an area of ongoing investigation. Lesioning is once again regaining interest, particularly with development of minimally invasive techniques such as laser interstitial thermal therapy and trans-cranial focused ultrasound. There are several methods for lead placement and procedural techniques will continue to evolve with time. A multidisciplinary team is critical for optimal patient evaluation, target selection, and postoperative followup. Medical ethics is a key part of the multidisciplinary management, particularly in case of children, patients with psychiatric disorders, and patients who are severely debilitated from their movement disorders.
Keywords: deep brain stimulation, functional neurosurgery, ethics
1.1 Introduction
Over the past three decades, deep brain stimulation (DBS) has become a widely used treatment for a variety of conditions since Benabid and colleagues first popularized the technique for the treatment of tremor. DBS systems can now be implanted using several different methods, with a range of options of stereotactic frames, image-guided targeting, and intraoperative microelectrode recordings (MERs) and testing. There are now multiple hardware and software options available for use in DBS, including different leads and implanted generators. A multidisciplinary team is critical to decide who is an optimal surgical candidate and what treatment strategy will be most suited for individual patient. Multidisciplinary collaboration maximizes the chance of successful DBS through appropriate preoperative evaluation of potential surgical candidates and continued postoperative care after DBS hardware placement. Medical ethics is an important part of the multidisciplinary management, particularly in case of children, patients with psychiatric disorders, and patients who are severely debilitated from their movement disorders.
1.2 History of Deep Brain Stimulation
Electricity has been a captivating possibility in treatment of human disorders for centuries, beginning with the earliest descriptions of treatment of pain with torpedo fish in Greek and Egyptian medicine, and investigations of contractions in frog muscle by Galvani.
For the next few decades after Horsleys resection of the precentral gyrus, attempts at treating movement disorders were aimed at interrupting the pyramidal motor tracts, but with a high degree of morbidity and mortality. Coopers approaches were intermittently successful and may have had a lower risk of complications than other prior open approaches. Though his work did little to advance technical refinements in the field of movement disorders surgery, his findings finally reduced further attacks on the descending cortical spinal tracts as a treatment for tremor.
Lesioning for psychiatric conditions also blossomed in the early to mid 20th century. Developments in neuroanatomy showed function could be localized to certain areas and anecdotal evidence of patients with frontal lobe damage and behavior changes led to a perception that psychopathology could be localized to the frontal lobes. Stereotaxy would allow a much higher level of precision in treating targets for psychiatric surgery.
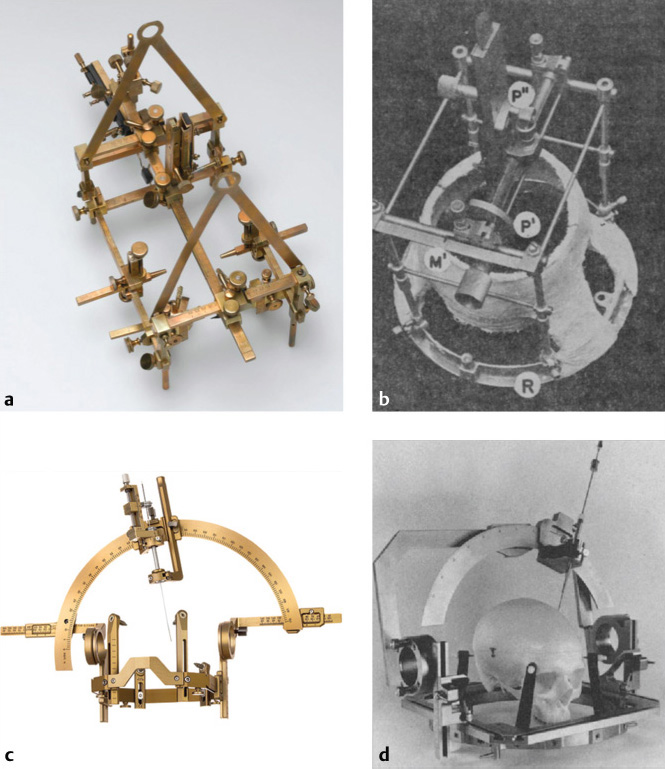
The development of stereotactic frames allowed more precise and safe neurosurgical procedures that had the potential to treat neurological diseases. Sir Victor Horsley collaborated with Robert Clarke to develop the first stereotactic frame ( The ablation procedures made possible with stereotactic surgery would lay a foundation to perform DBS for treatment of psychiatric illness. Both movement disorder surgery and psychosurgery led to the development of DBS.
The ablation procedures made possible with stereotactic surgery would lay a foundation to perform DBS for treatment of psychiatric illness. Both movement disorder surgery and psychosurgery led to the development of DBS.
Fig. 1.1 Stereotactic frames. (a) Horsley-Clarke frame (from the Science Museum, London).
(b) Spiegel-Wycis frame (from Spiegel et al.). (c) Leksell Coordinate Frame and Leksell Multipurpose Stereotactic Arc (Elekta, Inc).
(d) Cosman-Roberts-Wells frame (from Couldwell and Apuzzo).
Though the birth of modern DBS is typically attributed to Benabids 1987 paper on thalamic stimulation, neurosurgeons had been using acute stimulation long before that.
1.3 Ablative Procedures
Ablative procedures started to fall out of favor when DBS was introduced, but lesioning has remained an option for certain patients. Lars Leksells initial use of the Leksell frame included radiosurgical pallidotomies and thalamotomies, Though there is no current procedure that can supplant DBS, these new applications and methods of DBS will continue to be an active area of investigation.
1.4 Operative Techniques
DBS can be successfully performed in many different ways, with several options for targeting and hardware placement. Between centers, there is significant heterogeneity in how the procedure is performed, with differences in many elements of surgery including preoperative target and trajectory planning, frame usage, incision and burr hole planning, intraoperative clinical and stimulation testing, and postoperative imaging for confirmation.
1.4.1 Frame-based versus Frameless Approaches
Accurate targeting is critical to successful DBS. DBS can be performed with frame-based approaches and there are several frames available including the Leksell (
1.4.2 Microelectrode Recording and Intraoperative Monitoring
Another topic of debate is whether DBS performed with MER and intraoperative testing (awake) or DBS performed solely with anatomic/image-guided targeting (asleep) is more accurate and effective. There is some controversy regarding whether MER is an indispensable tool for accurate lead placement or current image-guided techniques are sufficiently accurate.
1.4.3 Description of Surgical Procedure
As described above, there are various methods of performing DBS, with new technology providing additional options that may make surgery more comfortable, convenient, safer, and more accurate. We will describe the surgical procedure for frame-based DBS, using MER and intraoperative stimulation. For other excellent reviews of surgical techniques, please see (Kramer et al)tomography (MRI/CT) localization without intraoperative recording or stimulation.
Preoperative planning
Patients are scheduled for a preoperative MRI, with thin-cut axial T1- and T2-weighted images as well as 3D volumetric T1 post-gadolinium-contrast images. Shortly before the surgical procedure, a CT scan with 1.5-mm axial slices at zero gantry angle is obtained. On the day of the procedure, a commercial computerized stereotactic planning station (e.g., FrameLink, Medtronic, Minneapolis, MD or iPlan Stereotaxy, Brainlab Inc., Westchester, IL) can be used to coregister the CT and MRI and plan the trajectory to the target. Fusion of MRI and CT helps in improving the spatial accuracy of targeting. Once target, entry point, and trajectory have been planned, the stereotactic planning station can be used to obtain X, Y, Z, and arc and ring angle coordinates.







 The ablation procedures made possible with stereotactic surgery would lay a foundation to perform DBS for treatment of psychiatric illness. Both movement disorder surgery and psychosurgery led to the development of DBS.
The ablation procedures made possible with stereotactic surgery would lay a foundation to perform DBS for treatment of psychiatric illness. Both movement disorder surgery and psychosurgery led to the development of DBS.