T1DM accounts for nearly 10% of DM cases and the incidence has slightly increased over time, with considerable variation by region and sampling technique [].
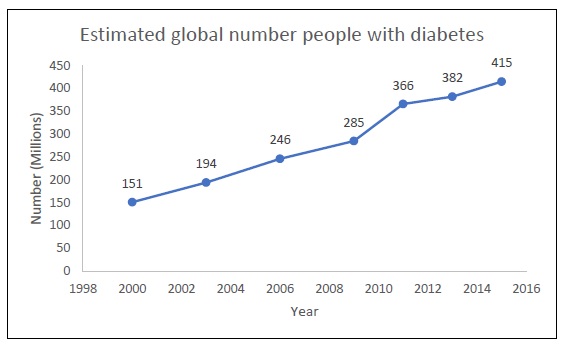
90% of all people with DM have T2DM, also known as adult-onset diabetes. As a result, global estimates of diabetes are predominantly reflective of change due to T2DM. T2DM is increasingly more common - likely due to the strong association with obesity, population aging, inactive lifestyle and poor dietary habits [].
Estimated number of people with diabetes over time worldwide (in millions) [].
The fallout from chronic hyperglycemia on the human body is accumulative over time. Morbidity and disability that arises from serious complications of diabetes include cardiovascular disease, kidney disease, neuropathy, limb amputation, and retinopathy. These complications, in turn, lead to an increased demand for medical care, reduce the quality of life, and place stress on families including financial burden. Altogether, diabetes-related care incurs an estimated $673 billion (12%) of global healthcare expenditure and 8% of all-cause mortality [].
Epidemiology of Diabetic Retinopathy
Ocular complications of diabetes include a spectrum of pathologies that range from refractive error and increased risk of cataract formation to cranial nerve palsies and blindness from diabetic retinopathy (DR) [].
Earliest estimates on the epidemiology of DR came from the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR). The WESDR was a population-based study conducted on a predominantly Caucasian cohort with both T1DM and T2DM in the 1980s. In this study, which has now accrued decades of follow up, it became possible to understand the increased risk of diabetic retinopathy progression over time [].
At the time of WESDR, it was not yet established that euglycemia was critical for risk factor modification in preventing retinopathy progression [].
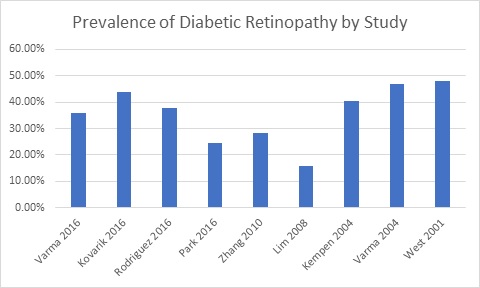
The prevalence of DR is widely varied due to variations in timing and characteristics of the snapshot of the defined population [].
Fig. (2)) The prevalence of diabetic retinopathy varies depending on the population characteristics and sampling techniques employed [].
The epidemiology of DME is of great interest due to its impact on quality of vision, but difficult to compare due to variations in definition of the disease. Studies vary with use of clinical examination, fundus photography and optical coherence tomography based definitions [].
Racial and ethnic impact on the epidemiology of DR is of great interest because of the wide differences in the reported rates of DR prevalence and the implications for environmental versus genetic influence. From the US, the third National Health and Nutrition Examination Survey (NHANES III) was a cross sectional study from the Center for Disease Control and Prevention from 1988-1994 to determine if racial and or ethnic differences modulated the risk of developing DR. This study demonstrated that Mexican-American participants had higher rates of DR compared to non-Hispanic white participants (33.4% vs 18.2%) [].
Genetics also contribute to susceptibility of DR onset and severity. Analysis of the Diabetes Control and Complications Trial (DCCT) indicates that glycemic control, as was reflected by hemoglobin A1c levels, was beneficial in reducing the incidence of DR [], The overall importance of genetics in determinants of diabetes related complications is an ongoing area of investigation.
Screening of Diabetic Retinopathy
Due to the asymptomatic nature of DR, individuals with diabetes should be properly screened for signs of DR and the progressive stages of DR. At a minimum, screening guidelines suggest a dilated fundus examination on an annual basis for T2DM and T1DM, beginning 5 years after diagnosis [].
Studies suggest that there is poor adherence to recommended guidelines such that an estimated nearly half of people with diabetes do not routinely receive an eye exam [].
CONCLUSION
Overall, type 1 diabetes represents a minority of cases of diabetes mellitus with indications that the disease is becoming slightly more common over time. Although people with T1DM have higher rates of ocular complications than people with T2DM, incident retinopathy has reduced with improved control of systemic management. In contrast, type 2 diabetes is much more prevalent, and the prevalence is increasing over time worldwide with substantial regional variation. Similar increasing trends are noted when examining the epidemiology of diabetic retinopathy.