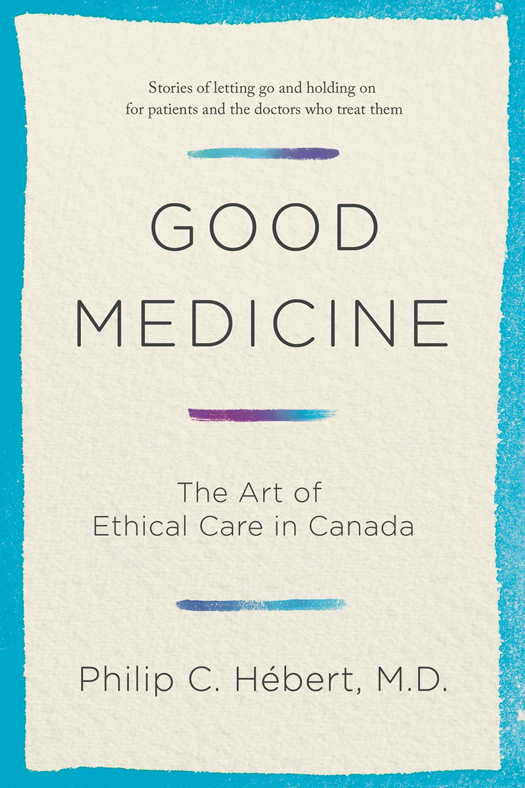
COPYRIGHT 2016 DR . PHILIP HBERT
All rights reserved. The use of any part of this publication, reproduced, transmitted in any form or by any means electronic, mechanical, photocopying, recording or otherwise, or stored in a retrieval system without the prior written consent of the publisheror in the case of photocopying or other reprographic copying, license from the Canadian Copyright Licensing Agencyis an infringement of the copyright law.
Doubleday Canada and colophon are registered trademarks of Penguin Random House Canada Limited
Library and Archives Canada Cataloguing in Publication
Hbert, Philip C., author
Good medicine : the art of ethical care in Canada / Philip Hbert.
ISBN 978-0-385-68325-8 (bound). ISBN 978-0-385-68326-5 (epub)
1. Medical ethics. I. Title.
R724.H394 2016 174.2 C2015-906227-6
C2015-906228-4
Cover images: J.D.S and Bariskina, both Shutterstock.com
Published in Canada by Doubleday Canada, a division of Penguin Random House Canada Limited
www.penguinrandomhouse.ca
v3.1
This book is dedicated to Dr. Nathan Kaufman (1915)
An extraordinary physician who knows the meaning of surviving well and flourishing against all odds
All changed, changed utterly.
W.B. Y EATS , Easter, 1916
CONTENTS
Introduction
STRANGERS IN A STRANGE LAND
W e all arrive as foreigners in the country of illness. Its flora and fauna, its language and customs are distinctive and challenging. The best guides for what can be a difficult and perplexing journey are knowledgeable and empathetic health care professionals. As there is almost always more than one path that patients might take, physicians, nurses, indeed all health care professionals must actively listen to patients and their loved ones so they can provide the best possible care. In turn, patients and their families must voice their concerns and openly share their stories so their health care professionals can understand how to best help them.
When it comes to serious illness, there is rarely an automatic passport allowing an easy entrance or exit. In modern medicine, the beginning or recognition of illness can be difficult. The end of illness can be complicated, too, and prolonged. The end is sometimes death, seen as a failure by many, as it sometimes is. But death may also come about through a process of consciously letting go. The challenge for allhealth care providers, patients, and familiesis to try to know when is the right time to do more and when is the time to let go. This book is partly about the process of letting go, but it is also about when we should not let go. It is about the experiences of patients and their families, and what we all should expect from a well-resourced health care system such as we have in Canada.
When Jane Mortimer was diagnosed with dementia in 2012, at the age of sixty-nine, she stated in what are known as advance instructions that she would not want extraordinary measures taken to keep her alive if she was unable to care for herself. Sadly, her dementia rapidly progressed, and she is now unable to speak or to feed herself. However, when offered food, she takes it, chews, and swallows. Despite Janes written instructions, the nursing home where she resides refuses to stop feeding her, saying that feeding is not considered extraordinary care. Janes family is unhappy with this situation and is uncertain what to do.
Gordie HoweMr. Hockey, one of the greatest hockey players of all timewas diagnosed with multi-infarct dementia (dementia caused by a series of strokes) at eighty-six years of age. Ravaged by his illness, he seemed lost, a shadow of his former self. He was virtually bedbound and had shed more than thirty pounds of his weight. His children, watching their father die little by little, in front of them, were unsure what to do. Gordies neurologist said there was nothing more that could be done for him. Then an American company with a site in Mexico offered Gordie a novel and untested treatment with stem cell therapy. His family wasnt sure whether to accept it or not. The company had offered the therapy for free. What have we got to lose? one son argued. Gordies neurologist was uncertain what to recommend. He had heard of such therapy but was worried about its dangers.
These scenarios are not uncommon in twenty-first-century medicine and will occur more and more frequently as our medical choices expand. In modern medicine we can almost always do things for patients. This is the era of medical miracles, after all. That does not mean we have a cure for some of the most serious diseases of the time, such as neurological illnesses like Huntingtons, Parkinsons, multiple sclerosis, dementia, and brain cancer. But we can, with effort, imagination, and money, help some patients to some degree.
Before the twentieth century, patients had very little say over their caredoctors orders held the day. Not that there was much for doctors to doother than chopping off gangrenous limbs or pulling teeth or draining abscesses. Most medical care was ineffective, if not (He added that patients were reassured just to see his father, and so he was, perhaps, his own strongest potion.)
Since then, science has radically and rapidly improved medical care. The black bag has become full of helpful drugsand even more magic. By the mid-twentieth century, real choices became available to patients. Paired with the proliferation of medicines scientific and technological advances were tremendous political and social shifts that caused medicine to tilt more positively in the patients favour. It was as a result of the vigorous human rights movements in the 1950s and 1960s that the idea of choiceand patient autonomywas fully recognized and came into rightful pre-eminence. The civil rights movement, the womens rights movement, the gay liberation movement, and the early AIDS movement, for example, all pushed medicine to adopt a more patient-oriented approach to decision making. Today there are alternatives of care that patients can consider, discuss, and choose between based on their own beliefs and desires. The idea of choice is a profoundly democratic one. It is bound up with notions of self-determination and privacy, and it represents an irresistible challenge to the authoritarian and paternalistic walls of traditional medicine.
Like many other professions, the medical profession has faced a loss of trust among the people it is meant to serve. This is, to some degree, a natural consequence of the evolution of medicine over the past century and the move away from its authoritarian roots. The nature of good medicine is changing, and this shift will leave some people happy and others dissatisfied. In my view, medical practitioners are responding to these challenges in largely positive ways. There is, for example, a deepened interest in understanding and preventing medical harm, and in basing treatment upon a critical understanding of what works and what does not. (Evidence-based medicine is a lot harder than you might think.) And beneath this is a constantly tested and renewed commitment among health care professionals to doing the best possible for their patients from the patients point of view.