Introduction
The skin is a vital organ for human life. It plays a complex set of functions and is essential for maintaining homeostasis. It covers the entire body surface providing the major site of interaction with the surrounding environment. The skins most important function is to maintain the hydric balance of the organism and form an effective mechanical barrier against external injury whether physical, chemical, or biological. Apart from protection, the skin actively participates in thermoregulation and it is involved in the immunological surveillance. It plays a critical role in the synthesis of vitamin D and functions as a sensory organ in detecting different stimuli (Ackerman ).
The skins health is determinant in social relationships. A compromised skin integrity results in a relevant psychological and social impact in peoples lives harming communication among individuals.
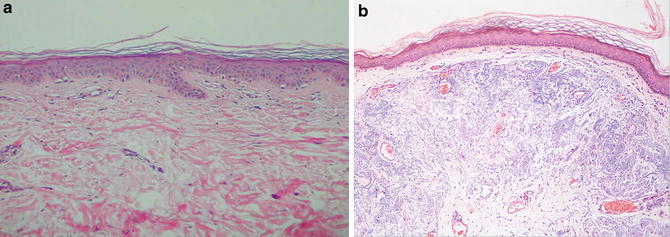
Cutaneous aging involves an intrinsic chronological process and also an extrinsic process due to environmental factors, especially sun exposure (Fig. ). A significant portion of the population is overly exposed to sunlight during labor and/or recreation activities. Damage of the ozone layer is an aggravating factor that contributes to earlier occurrence of signs of photodamaged skin on current population. At the microscopic level, a relevant feature of photoaging is the accumulation of solar elastosis in the upper and middle dermis. Avoidance of excessive sun exposure is still the most recommended strategy to prevent cutaneous photoaging.
Fig. 1
Eldery skin. ( a ) Elderly skin in an area unexposed to sunlight. Note that the epidermis is thin, with a flattened base, but there is no solar elastosis in the dermis. H&E, 100x. ( b ) Elderly skin in an area exposed to sunlight. Note that there are numerous basophilic fibers in the dermis named solar elastosis. HE, 100x
Moreover, the population is living longer and patients are seeking for low-risk cosmetic procedures with associated minimal downtime. Great advances have appeared in response to the aesthetic claims for treatments that will turn back the clock and make people look and feel younger.
The purpose of this chapter is to discuss the skins histology, physiology, and topographic particularities emphasizing on its important points for executing some cosmetic procedures. This step, along with the complete understanding of the mechanisms of action of established aesthetic treatments, is essential for safety and efficacy of these treatments.
The Epidermis
The structure of the skin consists of two layers: the epidermis and the dermis. The epidermis is the outermost layer of the integument. It is composed of stratified keratinized squamous epithelial tissue.
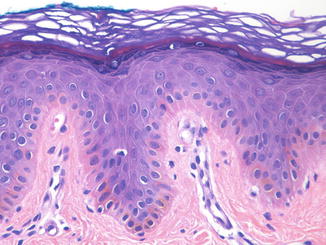
It is an avascular tissue that consists of four layers of keratinocytes in their various stages of differentiation. From the deepest layer to the more superficial, they are the basal cell layer , the spinous or squamous layer , the granular cell layer, and the stratum corneum . The first three compose the nucleated portion of the epidermis and are referred collectively as Malpighian layer. The stratum corneum is composed by completely keratinized cells that are no longer alive but still play an important role in the homeostasis of the epidermis (Fig. ).
Fig. 2
Epidermis. The epidermis is a stratified keratinized epithelium. The nucleated portion is composed by the basal cell layer, squamous cell layer, and granular cell layer, which are referred collectively as Malpighian layer. The stratum corneum is anucleated and composed by dead cells. (HE, 200x)
The interface between the two layers of the skin is known as the dermal-epidermal junction . It is an extremely complex structure and it is essential to life. The primary function of the basement membrane is to promote adherence of the epidermis to the dermis, keeping the permeability required for the diffusion of nutrients and oxygen. The basement membrane is not visualized in sections of tissue stained by hematoxylin and eosine, but it is seen as a thin line under the keratinocytes of the basal layer when Periodic acid of Schiff stain is applied.
Keratinocytes of the basal layer are the least differentiated cells of the epidermis and form a single row of columnar cells with the major axis perpendicular with the dermoepidermal junction. They are the only keratinocytes of the epidermis with reproductive ability, functioning as cell reservoir and supplying continuously, through cell division, keratinocytes to higher layers (stratum spinosum, stratum granulosum, and stratum corneum).
Depending on the bodys anatomical area , Malpighian layer thickness varies. In general, the thickness of the epidermis varies from 0.04 mm on the eyelids to 1.6 mm on the palms and soles of the feet. The spinous layer is composed by larger keratinocytes than the basal cells, with a polyhedric shape, and they may be arranged in five to ten layers of cells.
The granular layer has three rows of cells in the thin skin and is composed of large flattened cells, with a rhomboid shape and major axis parallel to the epidermis surface. Their cytoplasm is filled with keratohyalin granules that are quite basophilic. The keratohyalin granules contain substances such as pro-filaggrin (which is converted in filaggrin that functions as an adhesive promoting adhesion of keratin filaments to form thicker filaments) and loricrin (which contributes to the formation of an insoluble intracytoplasmic barrier known as cell envelope). The granulocytes also contain small lipid laminated granules known as Odland bodies. They are secreted to the extracellular environment during the keratinization process and contribute to maintain the stability, impermeability, and lubrication of the stratum corneum (Ackerman ).