Discussion
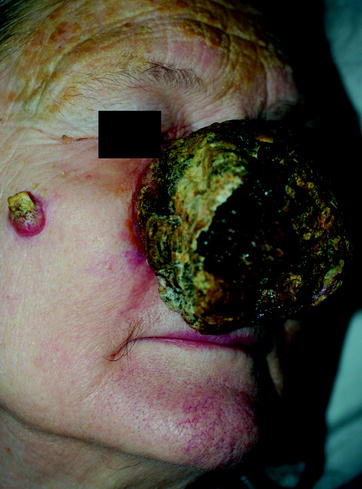
When is a dermatologist not a dermatologist? On vacation? At a family gathering? While exercising at the gym? At the theater or waiting for a subway? In reality, never. Dermatologists are skillful trained observers. Even without the antenna raised, they observe lesions and rashes on friends, relatives, and even complete strangers that in the context of an established doctorpatient relationship would demand attention and action, possibly urgently. But what should the dermatologist do when individual in question is not a patient and has not sought the doctors opinion? Should he or she offer an unsolicited diagnosis or advice? What if the consequences of inaction could be serious or even fatal for the patient?
Although offering an unsolicited medical opinion may be regarded as an act of beneficence, the physician does not have a strict moral obligation to do so [].
The degree to which the physician is morally obligated to act is affected by the seriousness and urgency of the risk to the individual, the degree of certainty of the diagnosis, and the presumption that the stranger would want the physicians opinion or intervention []. The more serious the consequences of inaction, the less certain the diagnosis needs to be before acting.
The obligation to bring a diagnosis to someones attention also depends on how obvious it is to that individual that something is wrong. In addition, one cannot assume that the person either knows how to access medical care or that the condition is even treatable. Unless the problem is treatable, there should be no obligation to offer an unsolicited opinion []. Indeed, offering an unsolicited diagnosis for a condition that is untreatable or for which no beneficial intervention exists could conflict with the physicians obligation of non-maleficence were the patient to suffer psychological distress or act in a self-destructive way.
A latent diagnosis that may remain so before causing harm imposes greater moral obligation upon the dermatologist. The bystander physician should possess appropriate medical knowledge to render an opinion, but need not be a specialist in the field. A psychiatrist can suspect a melanoma [] and a dermatologist can recognize exophthalmos as a sign of Graves disease or suspect a potential cardiac emergency.
Even where there appears to be a professional obligation or duty to offer unsolicited advice, ordinary morality (such as dont invade someones privacy) may clash with professional morality (the obligation to heal the sick and relieve suffering). Ones personal morals and ethics may conflict with ones professional duty and ethics [].
Ratzan [], to which anyone who has been present at a cardiac arrest can attest. The bystander role can be ambiguous. How severe or urgent is the situation? Is there a threat of harm increasing with time and resulting from the bystanders inaction? What are the bystanders ethical obligations? A professional is no ordinary bystander by virtue of technical or medical expertise and professional duties. An ordinary bystander may be a Good Samaritan while a physicians professional duty may create an obligation to stop and assist regardless of private morals. To what degree this applies to rashes and skin lesions is less clear than with a serious motor vehicle accident.
Table 1.1
The bystander phenomenon
| The bystander must notice that something is happening |
| Bystander recognizes it as an emergency or crisis demanding a response |
| Bystander attributes to self responsibility for acting |
| Bystander must decide on effective intervention |
| Bystander must decide how best to intervene |
Source : From Ratzan []
Having any sort of relationship with the individual may make it easier and seemingly less intrusive to offer a diagnosis or opinion. It is easier to strike up a conversation with someone with whom one has even a passing acquaintance. In addition, if the physician knows the individual, it might even make it possible to have a closer look at the lesion or rash without seeming overly intrusive.
As with any intervention, there are risks and benefits to be considered. These are summarized in Table . Intervention by the bystander physician can have unintended and unexpected consequences. For example, consider the following scenario. The physician notices a pigmented lesion on someones back at the beach and comments that it looks a bit worrisome and recommends that it be examined by a dermatologist. The person goes to his physician who remarks, youre lucky someone noticed that. It could have been very serious or even fatal if the diagnosis had been delayed a few more months. On the other hand, consider a different scenario: The same person goes to the dermatologist who tells him the lesion is nothing to be worried about. Based on the initial impression of the doctor at the beach, the patient is not fully reassured and insists on having the lesion removed. The wound dehisces, becomes infected, and heals with unsightly keloid scar. The two scenarios illustrate some of the potential risks and benefits of unsolicited diagnosis.