ABOUT THE AUTHOR
Dr. Samuel J. Mann is one of a relatively small number of physicians who specialize specifically in the treatment of hypertension. He is a professor of clinical medicine at the Hypertension Center of the New York Presbyterian HospitalWeill Cornell Medical Center, where he has a large consultation practice and is involved in hypertension research. He is the author of fifty scientific articles, a dozen book chapters, and a book, Healing Hypertension: A Revolutionary New Approach (1999). His recent research has focused on the management of hard-to-control hypertension, and on the role of the mind/body connection in understanding and treating hypertension.
In Hypertension and You, he focuses on what is wrong with how blood pressure medications are prescribed, and provides information and strategies that are not found in previous books. He explains how we can do much better in controlling hypertension and reducing the risk of stroke and heart attack, while reducing medication, side effects and costs, by using the right medications in the right patients.
INCORRECT BLOOD PRESSURE MEASUREMENT AND THE OVERTREATMENT OF HYPERTENSION
I t is not an overstatement to say that millions of people are on more blood pressure medication than they need because their blood pressure is measured incorrectly either at the doctors office or at home. Worse, in most cases, neither the doctor nor the patient is aware that the blood pressure is being overtreated.
In this chapter, I will present the most common errors that doctors make in measuring blood pressure in the office and that patients make in measuring their blood pressure at home. These errors usually lead to overestimation of blood pressure and to overtreatment. I will also convey the right way to measure the blood pressure, to avoid readings that are way off the mark.
Blood pressure has been traditionally assessed by measurement in the doctors office by the doctor or an assistant. Today, however, hypertension specialists and many internists rely more and more on home readings. The studies consistently show that your readings at home are better indicators of risk, and therefore a better guide to the need for treatment, than are office readings. I encourage most of my patients to check their blood pressure at home.
A monitor costs less than $100 and is clearly valuable and cost-effective. For example, you can determine whether or not you have white coat hypertension (i.e., elevated blood pressure in the doctors office) with normal readings at home. If you do, you might be able to reduce medication and medication costs.
Monitoring your blood pressure at home, you will need fewer visits to the doctor to check your blood pressure, reducing costs for you, for managed care organizations, and for Medicare. Will they reimburse you for the monitor? Probably not, although hopefully that policy is changing!
Another way to assess your home blood pressure is with a twenty-four-hour monitor, with a cuff placed on your arm at the doctors office and worn for twenty-four hours. Called ambulatory blood pressure monitoring, it is available in the offices of doctors who focus on hypertension. It automatically measures your blood pressure every twenty to thirty minutes over a twenty-four-hour period. It can tell your doctor your average blood pressure and how much it fluctuates. It also assesses your overnight blood pressure, which is at least as powerful an indicator of cardiovascular risk as is daytime pressure. Unfortunately, most health care plans and Medicare wont reimburse the cost, which is usually in the range of $250.
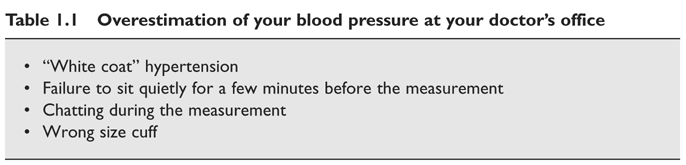
OVERESTIMATION OF YOUR BLOOD PRESSURE AT YOUR DOCTORS OFFICE
Table 1.1 lists the most common causes of overestimation of patients blood pressure in the doctors office. From what patients tell me, in this era in which doctors of necessity rush to see patient after patient, the most common error doctors make is taking the blood pressure measurement right away. They dont allow you to sit quietly for three to five minutes, as is the standard recommendation, to allow your blood pressure to settle down to its resting level. The result: overestimation of your resting blood pressure and overtreatment of millions of patients. It is a huge, yet ignored, problem.
Patients ask me whether the higher reading taken right away reflects a higher risk of developing hypertension or cardiovascular disease. The answer is no, usually not. It is normal for our blood pressure to be higher until we settle down for a few moments.
A second very common cause is chatting during the measurement. Your systolic blood pressure can increase 10 mm or more while talking, enough to affect treatment decisions. I enjoy chatting with patients, but I am rigid in insisting that they sit quietly before I measure their blood pressure. Is it okay if you are quiet and the doctor chats away? Probably.
A third common cause is the use of too small a cuff. If you have a large arm, whether from being overweight or from having a very muscular arm, the usual, standard size cuff might yield misleadingly high readings. A large arm cuff, which every doctor who checks blood pressure should have, solves the problem.
It is recommended that patients be seated in a chair with back support and feet on the ground, rather than on a doctors exam table with unsupported back and legs dangling in the air. The latter has been reported to produce higher readings. I must confess that I dont follow this recommendation, mainly because when I check the blood pressure in both positions, I find little difference in the readings. So is this recommendation important? Im not sure.
Other recommendations that are commonly violated are taking a single reading rather than at least three; deflating the cuff too quickly, which will yield a falsely low systolic and falsely high diastolic pressure; and rounding off to the nearest 5 or 10 mm.
The recommendations for how doctors should be measuring blood pressure were recently summarized in a report authored by the late Dr. Thomas Pickering.
White Coat Hypertension
Even if your doctor checks your blood pressure correctly, your readings could still be misleadingly high, a result of the alerting phenomenon in the doctors office. If your readings are elevated in the doctors office but are normal elsewhere, you could have what is widely known as white coat hypertension.
If your blood pressure is elevated at the doctors office but is truly normal at home, you are at lower risk of cardiovascular events than if your home readings were also elevated, and you might not need medication. But you must continue to monitor your blood pressure at home to make sure it remains normal, because individuals with white coat hypertension do have an increased risk of developing hypertension in the future. It is okay to ignore the high readings in your doctors office as long as you monitor your blood pressure at home, at least once a month.
Many patients and doctors wrongly believe that the white coat phenomenon can occur only if a patient feels very nervous when the doctor is checking his blood pressure. That is incorrect. It can also occur in patients who do not feel nervous. That is one more reason to check your blood pressure at home at some point before committing to lifelong medication.