Chapter 9
How vaccines work and their incredible impact
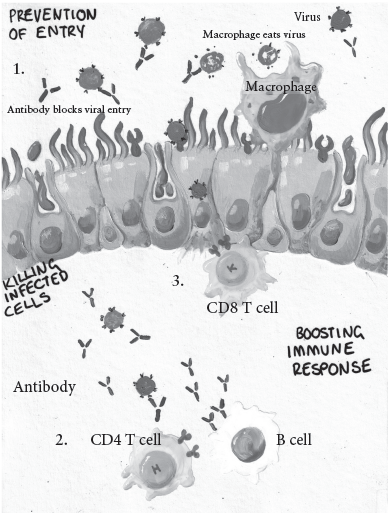
Two fields of science underpin vaccines: immunology and epidemiology. Vaccines are based around the principle that the immune system can remember things it has seen previously. In the days before vaccines, this meant that if you had been infected with something and survived you were unlikely to get that same infection again. Immunisation manipulates this system, producing a memory to an infection you are yet to see, without any of the bad bits of the infection itself. Having seen the vaccine, your B cells produce antibodies specific to the pathogen. This means that if you then come across the pathogen your blood is chock-full of protective chemicals that can recognise and kill it. Vaccination also gives you a small, highly focused army of T cells primed to hunt down and kill any infected cell (see figure 9).
The immune system works at an individual level. But vaccines are most effective as a population intervention, the fundamental principle being to reduce R , or the number of people that any one infected person will spread their disease onto: if R is less than 1 the epidemic contracts; if R is greater than 1 it spreads. Altering the dynamics of an infection with vaccines means you can protect the whole population without immunising the whole population. This population-level immunity is called herd immunity. Herd immunity even protects people who dont respond as well to the vaccine, for example the immunocompromised.
The percentage of the population that needs to be immune to achieve herd immunity varies the more infectious a pathogen is, the higher the vaccination rate needs to be. For a pathogen with a low R , such as Haemophilus influenzae B, you can reach herd immunity when only about 25% of the population are immune, but for pathogens with a high R like measles you need to immunise upwards of 90%. When applied properly, vaccine-induced herd immunity can be a potent tool. The vaccine against S. pneumoniae (sometimes called pneumococcus) is given to infants but provides two in one protection: the child doesnt get sick and it does not pass its germs on to its grandparents.
Epidemiological understanding of how pathogens spread also means vaccines can be focused on the correct populations. This builds on the point made in Chapter 3 that if you are never exposed to a pathogen then you dont need a vaccine against it. In a previous less-woke age, I would illustrate this with the Slappers and Nuns model, but now I probably should call it targeted vaccination but the principle remains the same. A vaccine against sexually transmitted infections will be more effective in people who are sexually active compared to those who have taken vows of celibacy.
Figure 9 How vaccines work: Vaccine protection is based on immune memory mediated by T and B cells. 1. Antibodies prevent infection they block the virus from getting into the cells. 2. The CD4 T cells boost the quality of the response. 3. CD8 T cells kill infected cells.
The population targeted for vaccination can be decided by the disease caused as well as the risk behaviour undertaken. In the UK the HPV vaccine was initially only given to girls, because the vaccine predominantly prevents cervical cancer, which is much harder to get if you dont have a cervix. It is now given to both boys and girls because it also prevents genital warts that can cause testicular cancer, infected boys can still spread the virus and the herd immunity benefit was not reaching into the MSM (men who have sex with men) community when only girls were vaccinated. The HPV campaign in the UK is one of the stories that highlights the remarkable power of vaccination. A very recent study showed a 90% reduction in cervical cancer since the introduction of the HPV vaccine: ten times fewer people got this type of cancer.
Celebration
And yet, despite the clear positive impact of vaccines, we live in an age, especially in richer countries, when people remain hesitant about their use. Before addressing why this might be the case, I think we need to celebrate the incredible success story of vaccination.
I always come back to the numbers. Lets start with the UK: in 1940 there were more than 60,000 cases of diphtheria, leading to 3,283 deaths. By 2002, vaccination had almost eliminated it with just two deaths from diphtheria between 1986 and 2002. Meningitis C, invasive pneumococcal disease, Haemophilus influenzae type B and rotavirus have been virtually eradicated. Polio and smallpox have both been completely eradicated.
These successes are reflected on a global level. The WHO estimates that vaccines against diphtheria, tetanus, whooping cough and measles prevent 23 million deaths every year. In 1963, when the vaccine was introduced, measles killed 2.6 million people a year; this has been cut globally to fewer than 100,000 which is still far too many. Likewise, childhood deaths from tetanus reduced from 800,000 in 1988 to 50,000 in 2013. This reduction of vaccine-preventable disease in the last twenty years is down to the efforts of multinational organisations such as GAVI (Global Alliance for Vaccines and Immunization) and support by governments and philanthropists such as Bill and Melinda Gates. The percentage of children under one who got at least one vaccination was 22% in 1980; it had increased to 88% by 2016.
If these everyday wins are not enough to persuade you, what about the big-ticket items? Lets start with polio. In 1981 there were about 460,000 reported cases of polio worldwide and in 2019 there were 545 cases, a thousand-fold reduction. In August 2020, bucking the trend for what was a pretty sorry year, Africa was declared free of wild type polio, meaning five out of six global regions are free of this disease. Only two countries now have wild type polio virus circulating: Afghanistan and Pakistan. If you compare the number of cases vs the world population (and admittedly this is not a globally spread risk) the chances of catching polio are one in two million, the same as tossing twenty-one heads in a row: in the USA you are considerably more likely to be injured on the toilet (22.5 cases per 100,000 population or a 1 in 5,000 chance).
There is a slight complication to this story. Africa is not completely free because live vaccine that has been pooped out can be infectious. Unfortunately, Sabins vaccine was not quite as stable as he thought. It is perfectly safe in the vaccinated person, but if left to its own devices in untreated sewage the virus can revert to a more virulent type viruses being tricky like that. There are now more cases of secondary infection from contaminated water than wild type virus but the numbers are vanishingly small for both. In 2019 there were 369 cases of vaccine strain-derived disease, compared to 176 of wild type virus. One of the pieces of good news that may have been overlooked in the deluge of misery that was 2020 was the emergency licensure in November of a new live attenuated polio vaccine. This new vaccine nOPV2, made by Bio Pharma in Indonesia has been genetically engineered to be more stable and will be deployed to prevent vaccine-derived polio infection. Hopefully this is the beginning of polios end.
Probably the biggest triumph of vaccines is the complete eradication of a pathogen. The best-known example is smallpox, rightly celebrated as a triumph of modern medicine. In 1959, the World Health Organization (WHO) started a campaign to eradicate the virus. The first attempt failed, mainly due to a lack of funding. A second intensified programme was launched in 1967, leading to the eradication of smallpox in South America in 1971 and Asia in 1975, leaving only Africa with cases of the virus. In 1977 Ali Maow Maalin, a Somali cook, was the last person to be naturally infected with smallpox. While he survived, the tale had a tragic twist. In 1978, Janet Parker, a medical photographer working at the University of Birmingham, contracted smallpox and died. How she came into contact with the virus is not clear; the lab on the floor below hers worked on the virus but smallpox cannot be transmitted through the air. The tragic death of Parker led to the global destruction of all stocks of the virus except for those at the Centers for Disease Control (CDC) in the USA and VECTOR, the alarmingly named equivalent in Russia (previously a hub for biological weapons research). Since 1978, there have been no cases of smallpox anywhere.