Infectious Burden: The Cause of Aging and Age-Related Disease
This book contains the ideas and opinions of its author. It is not in any way a substitute for the readers own physician(s) or other medical professionals based on the readers own individual conditions, symptoms, or concerns. If the reader needs personal medical, health, dietary, or other assistance or advice, the reader should consult a competent physician and/or other qualified health professionals. The author specifically disclaims all responsibility for injury, damage, or loss that the reader may incur as a direct or indirect consequence of following any directions or suggestions given in the book.
The unauthorized use and/or duplication of this material without the expressed and written permission of the author is strictly prohibited.
2016 by Michael Lustgarten. All rights reserved.
Cover Image: Scanning election micrograph of methicillin-resistant Staphylococcus Aureus (yellow) and a dead human neutrophil (red). Source: National Institute of Allergy and Infectious Diseases.
Introduction
We live in a microbial world. Although there are 7 billion people (7*10 ) on earth, in contrast, the total number of prokaryotes (including bacteria) and viruses have been estimated at 10 and 10 , respectively (Whitman et al. 1998; Duerkop et al. 2014). Even without including other microbes ( i.e. fungi, protozoa), were outnumbered by at least 10 to 1! Luckily, all of these microorganisms arent detrimental to human health, but more than 1400 microbial species have been shown to be pathogenic to people (Taylor et al. 2001).
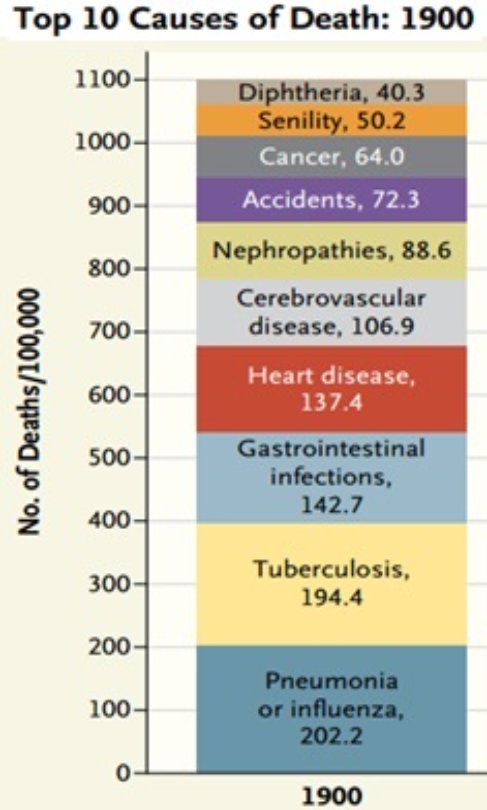
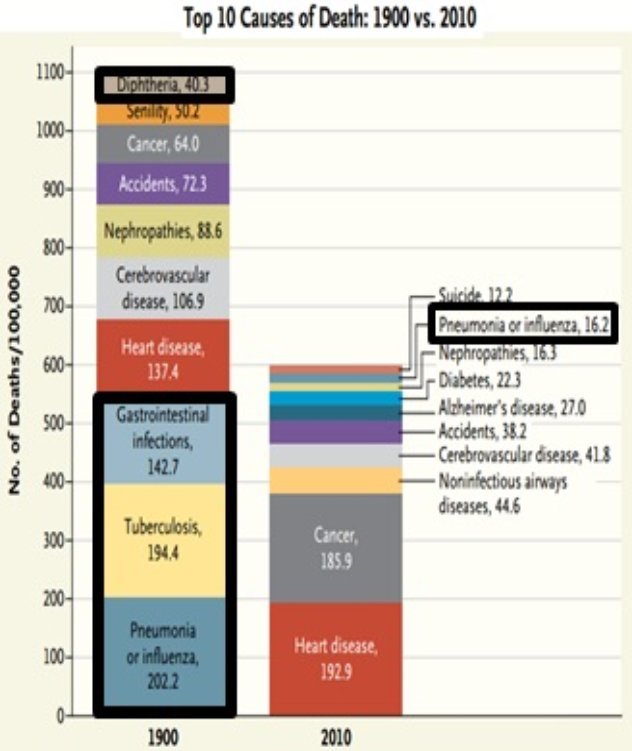
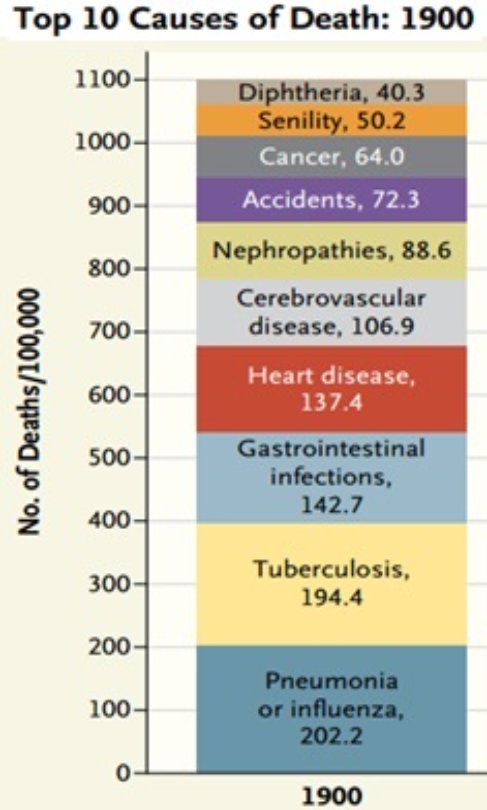
Accordingly, until ~1900, infectious diseases were the major cause of all deaths. As shown in the figure below, the infectious diseases, pneumonia/ influenza, tuberculosis, gastrointestinal infections, and diphtheria collectively accounted for 53% of all deaths (Jones et al. 2012):
As a result, lifespan was short, as people lived an average of only 30 years (Wiley 2005).
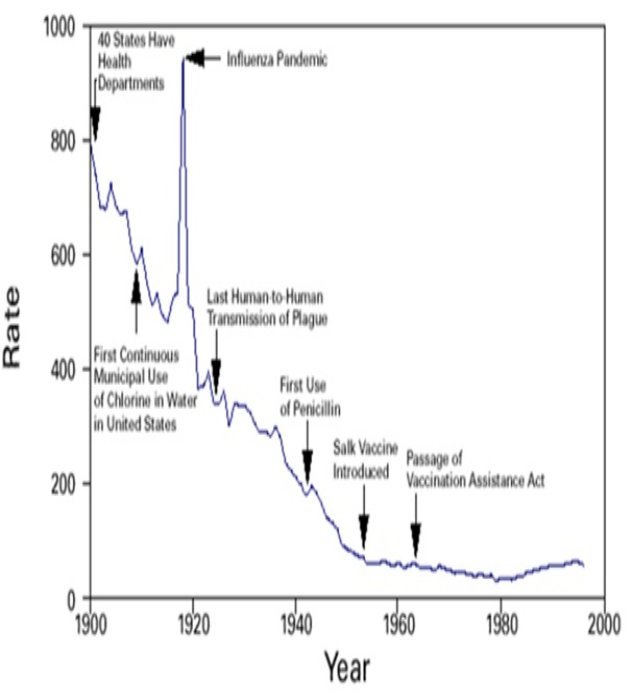
Over the next 100+ years, the establishment of public health departments that focused on sewage disposal, water treatment, food safety, organized solid waste disposal, and public education about hygienic practices, and the introduction of antibiotics and vaccines allowed for a dramatic decrease in infectious disease-related deaths ( http://www.cdc.gov ):
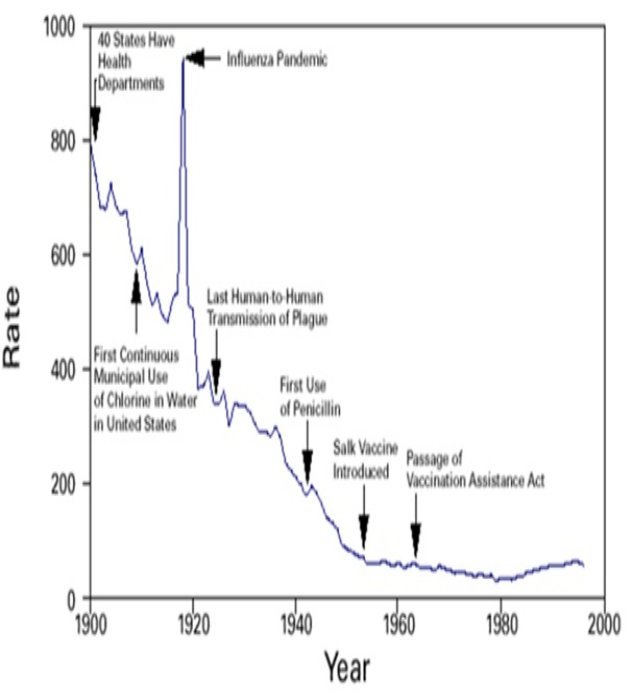
In 2010, deaths directly related to infectious diseases ( i.e. pneumonia/ influenza) were only 3% (Jones et al. 2012) of all deaths!
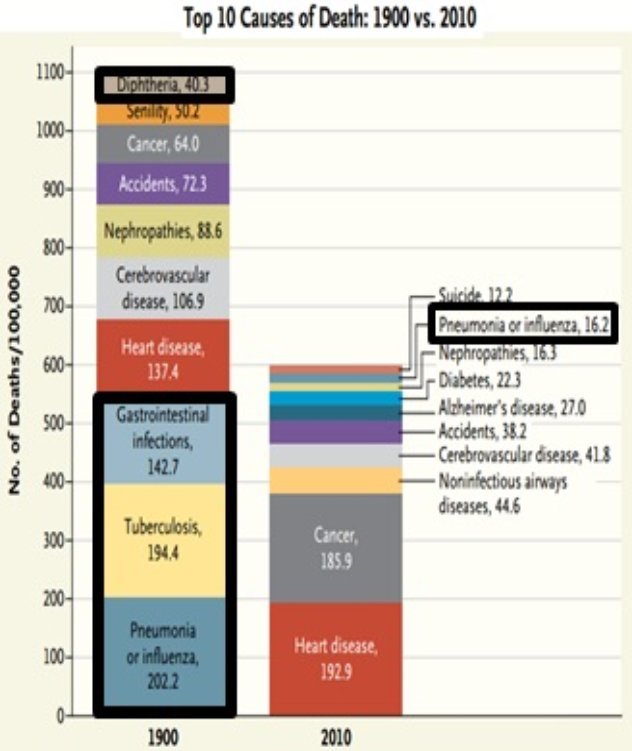
In addition, from 1900-2010, lifespan had its greatest increase in human history, as most people now live more than 70 years (Wiley 2005). This is the first line of evidence that links reductions in infectious disease-related mortality with an increased lifespan.
Because infectious disease-related mortality has been almost completely eliminated, can we say that the war against infectious disease is over?
Definitely not! Because we are heavily outnumbered by microbes, our existence is under constant attack. Eventually, our immune system cant properly handle this challenge, and very slowly, over time, more and microbes enter and live in inside us, where they accumulate in various tissues including blood vessels and the brain, thereby negatively impacting systemic physiology. This increases risk for most of the primary causes of death, including cardiovascular disease, cancer, Alzheimers disease, cerebrovascular disease, and diabetes. If we live long enough to escape those diseases, we once again succumb to infectious disease mortality, as pneumonia is the primary cause of death (other than old age) in adults older than 100 years. In sum, over the past 115+ years, we havent eliminated infectious-related mortality, we have merely delayed it!
Infectious Burden Underlies the Major Causes Of Death In 2016
Lets have a look at the data that supports the hypothesis that infection and the total sum of infectious microbes that live inside us (infectious burden) are involved with the etiology of the major causes of death in 2016.
Although it has long been thought that the blood is sterile and free of microbes, recent evidence disputes this hypothesis. In the figure below, we see that bacteria (measured by the presence of 16S rRNA on the y-axis) are found in whole blood (light grey bars), and within the sum of white blood cells, red blood cells and plasma (dark bars) in 29 young, healthy adults (average age, 21 years; Pass et al. 2016). On average, each subject had 40 million (4*10 ) circulating copies of 16S rRNA per milliliter of blood:

Each bacterium has 1 to 15 copies of the 16S gene per genome (Klappenbach et al. 2001) . When considering that our body contains about 5 liters of blood, this suggests a circulating bacterial load of 13 to 200 billion (low estimate, 4*10 *5/0.001 *15 = 13.3*10 ; high estimate, 4*10 *5/0.001 = 200*10 )!
We can also calculate how many circulating white blood cells (WBCs) are available to counteract this infectious burden. The WBC reference range is 4,000-11,000 cells per microliter of blood. Again, based on a total blood volume of 5 liters, we have 20 to 55 billion (low end of the range, 4000*5/ 0.000001 = 20*10 ; high end of the range, 11000*5/ 0.000001 = 55*10 ) circulating WBCs at a given time. At best, our WBCs outnumber circulating infectious microbes by approximately 4 to 1. At worst, our WBCs are outnumbered by 10 to 1!
Its important to note that the circulating bacterial load reported by Pass et al. (2016) was less for some and more for others. For example, subject #16 had ~2 million circulating 16S rRNA copies, whereas subject #26 had triple that amount, ~6 million.
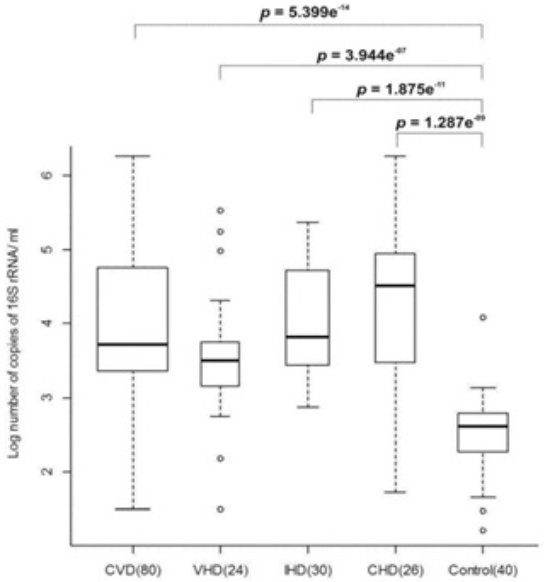
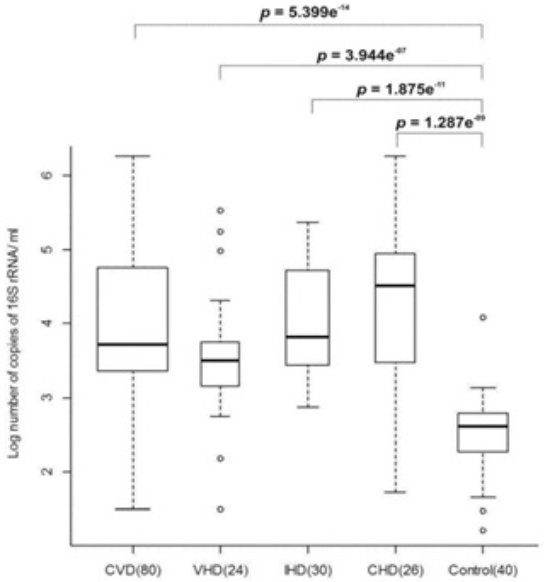
An increased level of circulating bacteria may be involved in the etiology of cardiovascular disease (CVD). As shown in the figure below, approximately 10-fold (log-scale) more circulating bacteria are found in CVD patients, when compared with healthy controls (Dinakaran et al. 2014). Even when dividing the CVD patients into subgroups of valvular heart disease (VHD), ischemic heart disease (IHD), and coronary heart disease (CHD), healthy controls still had significantly less circulating bacteria in their blood than each of the CVD subgroups:
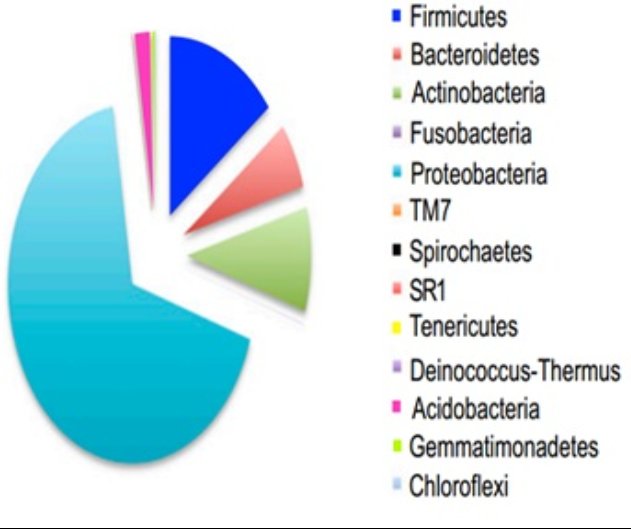
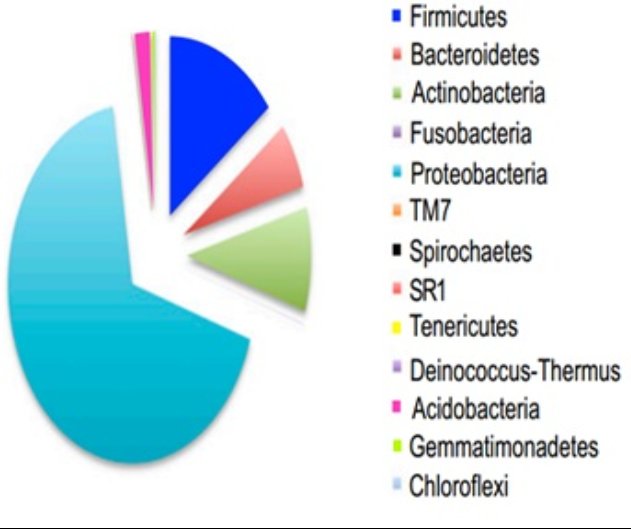
More specifically, increased blood levels of Proteobacteria but reduced Eubacteria (found within Firmicutes ) are associated with an elevated risk for future cardiovascular events, including myocardial infarction, myocardial ischemia, and coronary stenosis (Amar et al. 2013). Not only are circulating Proteobacteria increased in CVD patients, but they (and other various bacterial phyla) are found within atherosclerotic plaque (Koren et al. 2011). As shown in the image below, the predominant bacterial phyla found in atherosclerotic plaque are Proteobacteria (light blue), followed by Firmicutes (dark blue), Actinobacteria (green), Bacteroidetes (orange), and Acidobacteria (pink):
Many of the players related to atherosclerotic plaque formation, including C-reactive protein (CRP), LDL cholesterol, and fibrinogen (Spronk et al. 2004) have been shown to play a protective role against infection-related mortality. For example, 80% of wild type (WT) mice that are injected with Streptococcus pneumonae bacteria die within 2 days. However, in the presence of either 100 or 200 micrograms of CRP, survival (plotted on the y-axis) improves more than 4-fold (Mold et al. 2002):
Next page