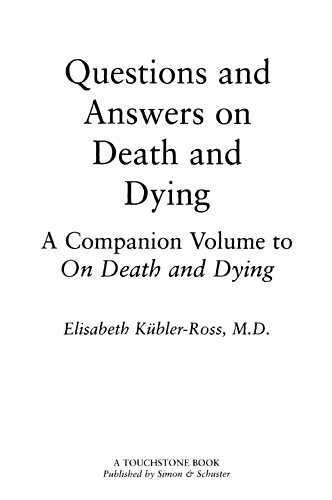
ELISABETH KBLER-ROSS IS THE AUTHOR OF
On Death and Dying
Questions and Answers on Death and Dying
Death: The Final Stage of Growth
To Live Until We Say Good-bye
Living with Death and Dying
Working It Through
On Children and Death
AIDS: The Ultimate Challenge
The Wheel of Life

TOUCHSTONE
Rockefeller Center
1230 Avenue of the Americas
New York, NY 10020
www.SimonandSchuster.com
Copyright 1974 by Ross Medical Associates S.C.
All rights reserved,
including the right of reproduction
in whole or in part in any form.
First Touchstone Edition 1997
T OUCHSTONE and colophon are registered trademarks of Simon & Schuster Inc.
Manufactured in the United States of America
The Library of Congress has cataloged a previous edition as follows:
Kbler-Ross, Elisabeth.
Questions and answers on death and dying / Elisabeth Kbler-Ross.
p. cm.
Previously published: Macmillan, 1974.
Includes index.
1. Death. 2. Terminal care. I. Title.
R726.8.K8 1993 93-9167 CIP
616.078dc20
ISBN 0-684-83937-7.
eISBN-13: 978-1-45166-446-1
DEDICATED TO
Manny, Kenneth, and Barbara, whose love makes this work possible
AND IN GRATITUDE TO MY FRIENDS:
Mwalimu Imara
Sheryl Rubin
Marge Lyons
Rosalie Monteleone
My two Alexian brothers, Frank and Gary,
and
Joe Baylyall of whom are always
there when I need them
Contents
Introduction
Since the publication of my first book, On Death and Dying (Macmillan, 1969), an increasing number of health professionals, lay people, and institutions have become involved with the needs of the terminally ill patient and his family.
Over the past five years I have participated in approximately seven-hundred workshops, lectures, and seminars on the care of dying patients. The participants came from every conceivable area of health care. There were physicians, members of the clergy, nurses, social workers, inhalation and occupational therapists, rehabilitation workers, ambulance drivers, funeral directors, as well as lay people who often had experienced the loss of a loved one. They came to seek answers to the many questions they brought with them.
This book is an attempt to answer some of the questions most frequently posed to me by audiences. Where they have been edited, it is only for clarification.
A book of this size can never answer all the questions. The most frequently asked questions regard the dying patient, and the largest portion of this book deals with patient-related issues. The next most frequently asked questions deal with staff problems and interdisciplinary teamwork. Special issues are covered in shorter chapters to make for easier reading.
I have specifically excluded chapters on Religion and Life after Death as well as chapters on Bereavment and Grief. This was done not only because of lack of space, but because there are others who are more qualified to answer these questions.
Again, as in my book, On Death and Dying, I have focused almost exclusively on the adult patient. Questions and answers relating to children are in my book, On Children and Death.
With the increasing number of inservice education programs for hospital personnel, seminars for medical students and other health professionals, and pastoral training centers, this book may stimulate discussion in areas where we have too often avoided the issuenot because we do not care, but because we feel so helpless in the face of the many unanswered questions arising at the time of this final crisis.
Questions and Answers on Death and Dying
1
The Dying Patient
The dying patient has to pass through many stages in his struggle to come to grips with his illness and his ultimate death. He may deny the bad news for a while and continue to work as if he were as well and strong as before. He may desperately visit one physician after the other in the hope that the diagnosis was not correct. He may wish to shield his family (or his family may want to shield him) from the truth.
Sooner or later he will have to face the grim reality, and he often reacts with an angry why me to his illness. If we learn to assist this angry patient rather than to judge himif we learn not to take his anguish as a personal insulthe will then be able to pass to the third stage, the stage of bargaining. He may bargain with God for an extension of life, or he may promise good behavior and religious dedication if he is spared more suffering. He will try to put his house in order and finish unfinished business before he really admits, This is happening to me.
In the depression stage he mourns past losses first and then begins to lose interest in the outside world. He reduces his interests in people and affairs, wishes to see fewer and fewer people and silently passes through preparatory grief. If he is allowed to grieve, if his life is not artificially prolonged and if his family has learned to let go, he will be able to die with peace and in a stage of acceptance. (Examples of these stages are described in detail in my book, On Death and Dying, (Macmillan, 1969).
The following questions come from patients and relatives, physicians and nurses, and hopefully allow the reader to identify with the patient and to feel more comfortable when he or she is faced with a similar problem.
TELLING THE PATIENT
When is the time for an attending physician to tell his terminally ill patient of his diagnosis?
As soon as the diagnosis is confirmed a patient should be informed that he is seriously ill. He should then be given hope immediately, and by this I mean he should be told of all the treatment possibilities. We usually then wait until the patient asks for more details. If he asks for specifics I would give him an honest, straightforward answer. I do not tell the patient that he is dying or that he is terminally ill. I simply tell him that he is seriously ill and that we are trying to do everything humanly possible to help him to function as well as he can.
Whose responsibility is it to inform the patient of his terminal illness? The doctor or the minister?
The doctor has the priority, but he may delegate this job to the minister.
Should every patient be told that he is dying?
No patient should be told that he is dying. I do not encourage people to force patients to face their own death when they are not ready for it. Patients should be told that they are seriously ill. When they are ready to bring up the issue of death and dying, we should answer them, we should listen to them, and we should hear the questions, but you do not go around telling patients they are dying and depriving them of a glimpse of hope that they may need in order to live until they die.
What can be done when the doctor refuses to tell the patient about his terminal illness? Do you suggest that someone else tell the patient? If so, who? Can he or she do it even without the doctors permission?
No, you cannot do it without the doctors permission. Unless the physician gives a minister or a nurse, or social worker the explicit request to do his job for him, it is inappropriate to do so unless you are the patients next-of-kin.
When does the patient begin to die and when, then, does our relationship begin to be one with a dying patient?
Next page