Stevo Duvnjak
Department of Radiology, Odense University Hospital, Odense, Denmark
ISBN 978-3-030-32164-2 e-ISBN 978-3-030-32165-9
https://doi.org/10.1007/978-3-030-32165-9
Springer Nature Switzerland AG 2020
This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed.
The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use.
The publisher, the authors, and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, expressed or implied, with respect to the material contained herein or for any errors or omissions that may have been made. The publisher remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This Springer imprint is published by the registered company Springer Nature Switzerland AG
The registered company address is: Gewerbestrasse 11, 6330 Cham, Switzerland
Preface
Endovascular aortic repair has revolutionised the treatment of patients with abdominal aortic aneurysms. However, frequent occurrence of endoleaks and the risk of rupture during long-term follow-up are issues that still need to be resolved. There are a lot of data on endoleak treatment, showing that endoleak recurrence and the risk of rupture in the long term are greater after endovascular repair than after open surgery. Patient selection is of the utmost importance, and every time we treat a patient with challenging anatomy outside the instructions for use of endovascular repair, the risk of endoleaks increases. We can achieve a satisfactory result in the short term, but problems will occur during follow-up. Today, our patients live longer, and so the treatment we provide needs to meet that requirement.
This book is the result of my personal commitment and dedication to endovascular aortic repair, and it presents cases treated by me. The book is intended to describe techniques for endoleak treatment not as the only possible ways to tackle endoleaks but, rather, as supplements to all other possible techniques. The book presents cases involving different types of endoleaks, from simple to complex, and interventional techniques are described to provide practical help for colleagues who treat such cases. There is an absolute need to improve knowledge and mastery of techniques for use of different embolisation materials. Colleagues in different specialities may find this book interesting, such as interventional radiologists, vascular surgeons, cardiologists and others.
I would like to thank all of my colleagues in the vascular radiology and vascular surgery departments at Odense University Hospitalincluding doctors, radiological technicians, nurses and all other stafffor helping me to successfully complete this project. Today, we all need good teamwork to make a difference.
Stevo Duvnjak
Odense, Denmark
2019
Springer Nature Switzerland AG 2020
S. Duvnjak Endovascular Abdominal Aortic Repair- Endoleak Treatment https://doi.org/10.1007/978-3-030-32165-9_1
1. Endoleak Classifications
Stevo Duvnjak
(1)
Department of Radiology, Odense University Hospital, Odense , Denmark
Stevo Duvnjak
Keywords
Endoleak Types of endoleak EVAR Complications Endoleak treatment
1.1 Endoleak Classifications
An endoleak is defined as persistent perfusion of an aortic aneurysm after endovascular treatment with an abdominal stent graft []. Endoleak type I occurs when the sealing zone is not adequate at either the proximal or the distal attachment site.
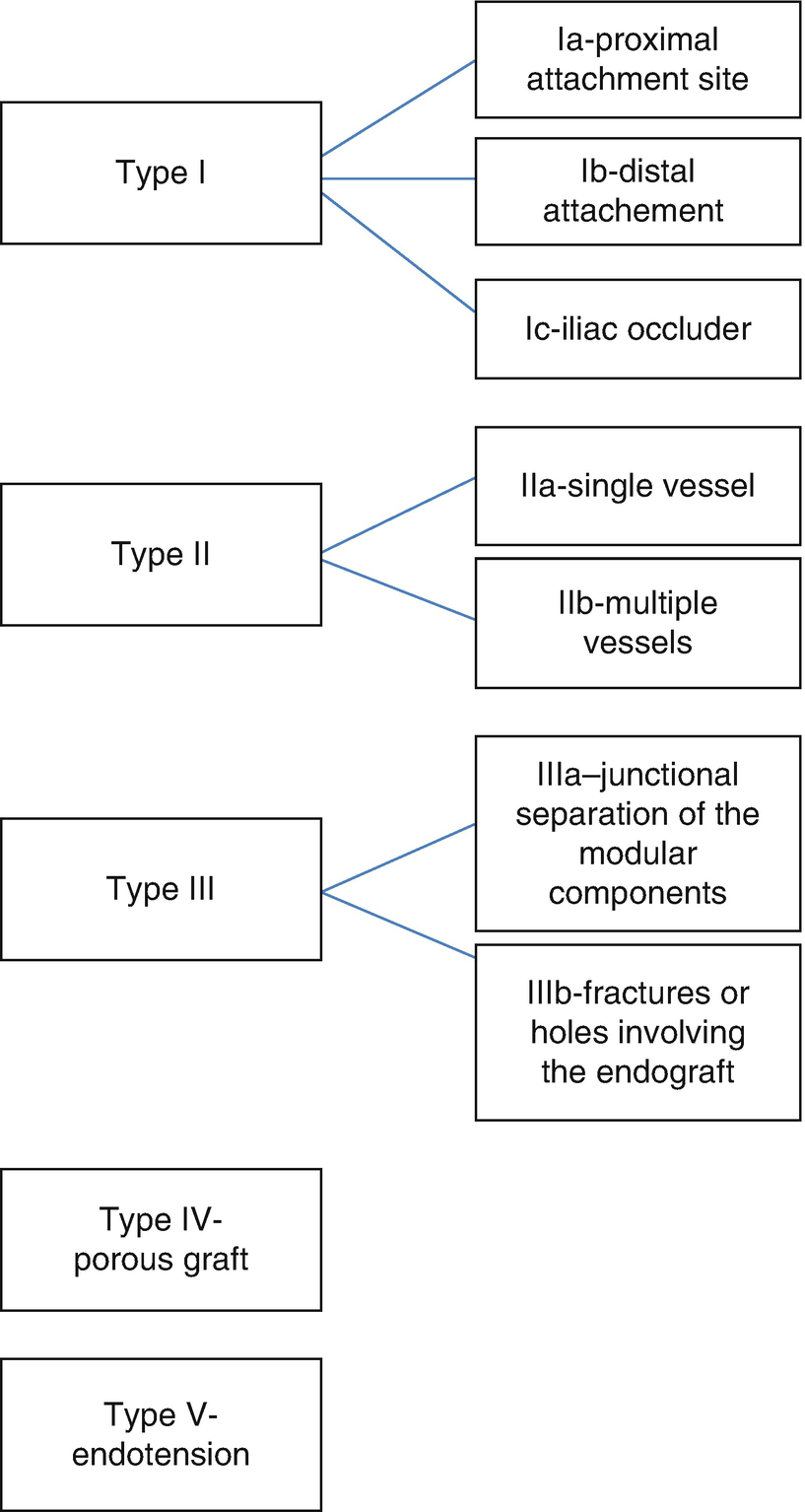
Fig. 1.1
Schematic overview of different types of endoleak
Calcifications, the length of the landing zone and angulation of the aortic neck or iliac vessels, an undersized or excessively oversized stent graft and a problem with deployment of the stent graft are frequent causes of endoleak type I occurrence. Endoleak type II is the most frequent type of endoleak and occurs via retrograde filling of the aneurysm, usually through the inferior mesenteric artery and lumbar arteries. In some cases, an accessory renal artery or the sacral median artery causes this type of endoleak as well. Endoleak type III occurs because of inadequate overlapping between the stent graft components, separation of the components or fabric tears. Endoleak type IV is due to porosity and in todays grafts, it is very rare in practice and is self-limited. Endoleak type V (endotension) is defined as enlargement of the aneurysm without detection of any other type of endoleak. There is some ongoing debate that endoleak type V is another type of endoleak that cannot be seen during imaging surveillance. Endoleak type I and type III are high-pressure endoleaks and need some intervention in all cases. There are publications reporting that some type Ia endoleaks can spontaneously disappear [].
Endoleaks can be seen in 2050% of patients treated with an endovascular repair [].
The initial treatment for endoleak type Ia is balloon angioplasty with a compliant aortic balloon (1046 mm), advanced through a 12 French (12 Fr) sheath [].
Treatment of endoleak type Ib or type Ic is much simpler and usually requires additional stent graft deployment, balloon angioplasty or, in some cases, embolisation. If the landing zone is in an external iliac artery, the internal iliac artery needs to be occluded to avoid endoleak type II [].
Treatment of endoleak type IIIa and type IIIb is usually straightforward with additional stent graft extension. In some cases, aorto-uni-iliac stent graft configuration and a crossover bypass are needed. There is a special bifurcated stent graft with a short body that can be used to avoid a crossover bypass, but the time to production is a few weeks [].