Editors
Valentino Cherubini , Daniela Elleri and Stefano Zucchini
Glucose Sensor Use in Children and Adolescents
A Practical Guide
Editors
Valentino Cherubini
Department of Womens and Childrens Health, Azienda Ospedaliero-Universitaria Ospedali Riuntiti Ancona, G. Salesi Hospital, Ancona, Italy
Daniela Elleri
Endocrine/Diabetes Department, Royal Hospital for Sick Children, Edinburgh, UK
Stefano Zucchini
Pediatric Endocrine Unit, Department of Woman Child and Urologic Diseases, S.Orsola-Malpighi Hospital, Bologna, Italy
ISBN 978-3-030-42805-1 e-ISBN 978-3-030-42806-8
https://doi.org/10.1007/978-3-030-42806-8
Springer Nature Switzerland AG 2020
This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed.
The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use.
The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. The publisher remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This Springer imprint is published by the registered company Springer Nature Switzerland AG
The registered company address is: Gewerbestrasse 11, 6330 Cham, Switzerland
Preface
Technology is nowadays an integrated part of day-to-day diabetes management, and an increasing number of patients are currently using continuous glucose monitoring (CGM) devices and smart insulin pumps.
Over the last few decades, significant progress has been achieved in terms of systems performance and convenience of use. Manufacturers are continuing to update existing technologies so that new devices are regularly becoming available on the market.
Both patients and healthcare professionals must therefore keep up-to-date with these technological advances to provide the best care.
The suboptimal performance of the first CGM devices has initially been seen as the weakest link in the development of closed loop systems, but the latest CGM models have improved and reached sufficient accuracy to allow the development of semi-intelligent insulin pumps.
Childrens diabetes care has specific challenges including greater glucose variability, hypoglycemia unawareness, and other unpredictable factors such as variable eating patterns. For these reasons, children may get the greatest benefit from the use of technology.
This booklet represents a practical guide in explaining how CGM devices work, their use in children with type 1 diabetes, their benefits, and possible pitfalls. The booklet also contains several practical pictures, which would hopefully help getting familiar with the use of different types of devices.
The authors of this booklet have longstanding clinical experience in caring for children with diabetes and contributed to the scientific knowledge in the field. The booklet is aimed at all caregivers willing to develop a practical knowledge on currently available CGM devices used in children with type 1 diabetes.
Valentino Cherubini
Daniela Elleri
Stefano Zucchini
Ancona, Italy Edinburgh, UK Bologna, Italy
Contents
Stefano Zucchini
Chetty Tarini
Giulio Maltoni and Stefano Zucchini
Valentino Cherubini
Chetty Tarini
Daniela Elleri
Giulio Maltoni
Anna Maria Paparusso
Daniela Elleri
Maria Cristina Alessandrelli
Valentino Cherubini
Springer Nature Switzerland AG 2020
V. Cherubini et al. (eds.) Glucose Sensor Use in Children and Adolescents https://doi.org/10.1007/978-3-030-42806-8_1
1. Introduction on Use of Technology in Pediatric Type 1 Diabetes
Stefano Zucchini
(1)
Pediatric Endocrine Unit, Department of Woman Child and Urologic Diseases, S. Orsola-Malpighi Hospital, Bologna, Italy
Diabetes mellitus is a chronic disease affecting millions of people worldwide. Type 2 diabetes is the most frequent form, involving more than 10% of the population over the age of 50 in some developed countries and it is mainly associated with sedentary habits and obesity. Type 1 diabetes (T1D) represents 510% of the cases of diabetes and affected individuals need insulin therapy right from diagnosis. Type 1 diabetes most commonly affects children and young people as it is diagnosed before the age of 18 in over 50% of cases, thus exposing the subjects to hyperglycemia for several decades. Chronic hyperglycemia , whatever the cause is, inevitably leads to the typical diabetes complications affecting both the microvascular circulation mainly of the retina, the kidneys and peripheral nervous system, and the big vessels, therefore accelerating atherosclerotic processes. Myocardial infarction is the first cause of death in patients suffering from any types of diabetes.
The incidence of T1D is increasing at the rate of about 4% per year, therefore it is estimated that new cases will double in 20 years, with preschool children showing the higher increase in incidence []. At the moment, there is no immediate prospect of a cure and lifelong insulin therapy is required.
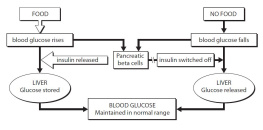
One of the main aims of diabetes treatment is to keep blood glucose (BG) levels within a specified range: the desirable target is between 70 and 180 mg/dL, therefore preventing hypoglycemic episodes (glucose <70 mg/dL), as well as prolonged hyperglycemic excursions leading to diabetes complications. If over 60% of time is spent within this target, mean BG is likely to be around 150 mg/dL, equivalent to an HbA1c level of 7% (53 mmol/L). Most international recommendations indicate a value less than 7% as ideal in adults and presently less than 7% also for children [].
The key treatment of T1D consists in balancing insulin doses with food, physical activity, and lifestyle. Starting from the 1980s, BG levels could be measured at home by finger pricking for the first time, which made the link between insulin dose and BG, food, and exercise easier to understand. As a consequence, structured education with empowerment of patients and families became the milestone of diabetes treatment. The appearance of new insulins, both rapid and long-acting analogues, on the market from the 1990s and the introduction of carb-counting techniques from the year 2000, completed the puzzle of the modern treatment to be adopted for every patient with T1D. Basal bolus treatment with insulin analogues or with insulin pumps, associated with carb-counting, is currently the most recommended approach to T1D therapy and management. Despite these recent technological advances, mean HbA1c levels often remain elevated in young patients with T1D []. Psychological factors and the burden of diabetes management may play a role and negatively impact glycemic outcomes.