Michael Y. Henein (ed.) Valvular Heart Disease in Clinical Practice 10.1007/978-1-84800-275-3_1 Springer-Verlag London Limited 2009
1. The Mitral Valve Disease
Abstract
Common causes of heart valve disease are rheumatic, calcific and less frequently congenital. With the significant decline in the incidence of rheumatic fever in Europe and North America over the last 50 years a parallel shift in the etiology of valve disease occurred with a fall in the incidence of rheumatic valve disease and an increase in the prevalence of degenerative valve pathology. Rheumatic valve disease, however, remains prevalent in the developing countries in Africa, South America and parts of Asia, particularly in areas with limited clinical services. The commonest valve involved with rheumatic pathology is the mitral valve, but this is not exclusive since aortic and tricuspid valves can also be involved [1]. The apparent contemporary increase in the diagnosis of valve disease results from the global increase in age of the population as well as the easy availability and routine use of echocardiography in cardiology clinics
Common causes of heart valve disease are rheumatic, calcific and less frequently congenital. With the significant decline in the incidence of rheumatic fever in Europe and North America over the last 50 years a parallel shift in the etiology of valve disease occurred with a fall in the incidence of rheumatic valve disease and an increase in the prevalence of degenerative valve pathology. Rheumatic valve disease, however, remains prevalent in the developing countries in Africa, South America and parts of Asia, particularly in areas with limited clinical services. The commonest valve involved with rheumatic pathology is the mitral valve, but this is not exclusive since aortic and tricuspid valves can also be involved []. The apparent contemporary increase in the diagnosis of valve disease results from the global increase in age of the population as well as the easy availability and routine use of echocardiography in cardiology clinics. Age affects the valves by making the leaflets thick with fibrous strands and adipose tissue deposition at the closure lines as well as increased calcium deposition. Isolated myxomatous changes may also occur in the valve fibrosa. This complex pathology eventually results in valve dysfunction. In an echocardiographic examination, such effects of age on valve leaflets should be carefully considered, particularly in patients with a suspected diagnosis of endocarditis since leaflet thickening may appear like small vegetations. They should also be distinguished from other small benign tumors, e.g., fibroelastoma.
Medical treatment of mild valve disease is limited, focusing mostly on prophylaxis against endocarditis. In more significant valve disease, medical treatment aims at optimizing the hemodynamics and consequently protecting against ventricular dysfunction. Surgical correction of valve disorder is the main conventional treatment of severe valve disease, particularly in patients with maintained ventricular function. Those with additional irreversible ventricular dysfunction may face significant surgical risk, thus medical therapy might be the best management option for them. In general, valve-related mortality is more prevalent in aortic valve disease than mitral valve disease, largely due to either sudden death from arrhythmia or the frequent development of left ventricular dysfunction that causes congestive heart failure. Other causes of death in valve disease are additional pathologies, e.g. coronary artery disease, endocarditis or arrhythmia. Overall valve surgery is 510 times less frequently performed than that for coronary artery disease [].
Normal Mitral Valve Anatomy and Function
Optimum function of the mitral valve depends on the integral function of all its components: leaflets, chordae, annulus and papillary muscles in addition to the left atrium and the left ventricle. A normal mitral valve does not close passively. In addition to the pressure difference between the ventricle and the atrium in systole, the annular contraction and papillary muscle contraction play an important role in the competence of the mitral valve. The anterior mitral valve leaflet represents a continuation of the posterior aortic root wall. The D-shaped annular fibrous ring is located mainly posteriorly, although significant variability exists in different individuals. The normal diameter of the mitral annulus is approximately 3 cm with a circumference of 89 cm. The annulus is not a passive structure, so in addition to its normal movement towards the apex in systole, the contraction of the posterior myocardial muscle shortens its diameter by 25%, making annular dynamics a very important component in the mechanism of mitral valve competence. Left atrial cavity enlargement and shape change result in mitral annular dilatation and hence overall valve dysfunction and incompetence. With progressive increase in left atrial size and development of atrial fibrillation, the lost mechanical atrial activity significantly contributes to mitral valve incompetence and the development of mitral regurgitation. Likewise, atrial fibrillation itself has been shown to contribute to the enlargement of the left atrium and consequently, the development of mitral regurgitation. The two leaflets of the mitral valve meet at the medial and lateral commissures. The U-shaped anterior leaflet area is larger than the posterior leaflet by approximately 34 cm2. The posterior leaflet is, however, wider and shorter than the anterior leaflet by approximately 1.5 cm2. The posterior leaflet is made up of a number of scallops, commonly three. The two leaflets coapt at the zone of apposition leaving an overlapping segment 5 mm long. The chordal anatomy of the mitral valve is complicated, with around 12 primary chordae rising from each papillary muscle, which divide into secondaries and numerous tertiary branches which attach themselves to the margins of the two leaflets. In addition, a number of basal chordae also attach themselves to the ventricular surface of the two leaflets and to the commissures. The location of the chordae follows that of the papillary muscles antero-laterally and postero-medially. Any rupture or redundancy of the chordae or extra tissue in the leaflets results in mitral regurgitation.
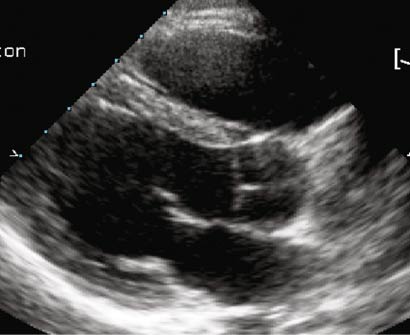
The normal mitral valve orifice cross-sectional area is approximately 5.0 cm2, Figure .
Figure 1.1.
Parasternal 2D long axis view showing anterior (extending from the posterior aortic wall) and posterior (extending from the left atrial posterior wall) mitral valve leaflets.
Figure 1.2.
Transmitral Doppler flow velocities from a young subject showing dominant early diastolic component ( top ) and an elderly showing dominant late diastolic component ( bottom ).
Mitral Stenosis
Congenital mitral stenosis : It is a relatively rare group of anomalies with considerable variations in the morphological features. Normally included in this diagnosis are cortriatriatum and supra-valvar mitral membrane, which can be identified from the four-chamber and long axis cross-sectional images Figure . Characteristically, color flow Doppler reveals acceleration proximal to the mitral valve leaflets. It is not unusual, however, for the supra-valvar mitral stenosis to be associated with thickened mitral valve leaflets and chordal abnormalities. It is unusual to find isolated mitral valve stenosis. In addition to thickened and dysplastic leaflets, anomalies of the chordae and the papillary muscles may be seen. In the classical parachute mitral valve, all the chords insert into a single papillary muscle.