PART ONE
INTRODUCTION
PART TWO
DEVELOPING AN EVIDENCE-BASED CULTURE
PART THREE
LOCATING THE EVIDENCE
PART FOUR
HOW TO EVALUATE CLINICAL PRACTICE
PART FIVE
TRANSLATING EVIDENCE INTO PRACTICE
USING EVIDENCE TO GUIDE NURSING PRACTICE
2e
Mary Courtney
Helen McCutcheon
CHURCHILL LIVINGSTONE
CHAPTER 1 Evidence-based nursing practice
Mary Courtney, Claire Rickard, Joy Vickerstaff, Anthea Court
1.1 Learning objectives
After reading this chapter, you should be able to:
1. understand what evidence-based practice (EBP) is
2. understand the benefits and alternatives to using EBP
3. explain what has caused the major spread of the EBP movement
4. list where evidence may be located to support best practice
5. describe two major structures promoting the utilisation of EBP in Australiathe National Institute of Clinical Studies (NICS) and the Joanna Briggs Institute (JBI)
6. explain how evidence may be incorporated into nursing practice, and
7. discuss the challenges the EBP-based movement has posed for both nursing education and nursing research.
1.2 Introduction
This chapter introduces the reader to the development of the evidence-based practice (EBP) movement and provides an overview of why EBP has spread so rapidly over the past 15 years. It explains how evidence may be incorporated into nursing practice and examines the challenges the EBP-based movement has posed for both nursing education and nursing research.
1.3 What is evidence-based practice?
Health professionals currently advise their patients to stop smoking. Why do they give this advice? Why dont they advise them to start smoking or increase their smoking intake? The reason is that evidence is available which demonstrates:
high levels of smoking are associated with increased risk of lung cancer, and
stopping smoking reduces the risk of lung cancer.
This is an example of evidence that can identify the cause of a disease and the effectiveness of an intervention to improve patient outcomes and decrease illness and disability.
).
).
:2) published the first textbook on evidence-based medicine and defined it as:
The conscientious, explicit and judicious use of current best evidence in making decisions about the healthcare of patients.
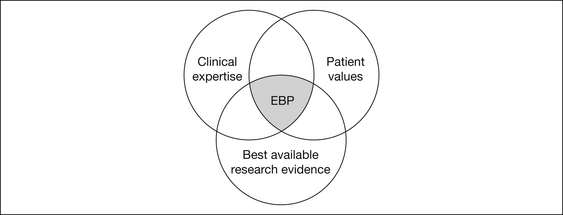
also included patient values as well as clinical expertise:
The practice integrates clinical expertise and patient values with the best available research evidence.
).
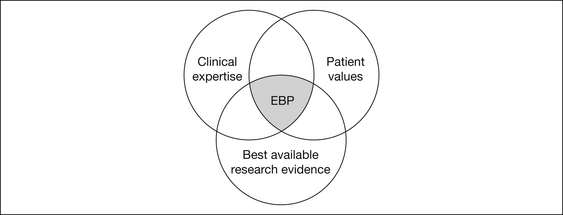
Figure 1.1 The three elements of evidence-based practice
Source:
).
1.4 What are the benefits of evidence-based practice?
There are benefits of EBP for patients/consumers, nurses, healthcare organisations and the community.
1.4.1 For patients/consumers
To healthcare consumers, it may seem ludicrous, or even frightening, that the EBP concept is relatively new. Patients typically accept recommended care from health professionals with the unspoken assumption that the practitioner knows what works.
1.4.2 For nurses
In an ideal world, nurses could keep up to date by reading all of the published literature in their relevant area. In reality, with approximately a thousand new publications each year relevant just to surgical nursing, for example, this is clearly an impossible task. EBP allows a more structured and streamlined way of keeping abreast of relevant new developments without becoming overwhelmed by information overload.
EBP also allows nurses to communicate effectively with their patients and with the healthcare team about the rationales for decision making and care plans. An EBP nurse is a confident professional, feeling assured that they are providing care which is supported by facts rather than habits, and can take legal accountability for their practice.
1.4.3 For healthcare organisations
A commitment to EBP philosophy allows healthcare organisations to position themselves in the market as quality institutions. An EBP-compliant institution should be less likely to attract litigation, and will be able to successfully defend the care delivered if it was in line with international best evidence at the time of care. In addition, EBP allows the scrutinising of practice for effectiveness. This process often results in practice changes that allow significant cost savings, or alternatively justify necessary additional expenditure. This is attractive to organisations frequently struggling to meet assigned budgetary limits, or lobbying government for additional funds.
1.4.4 For the community
Through the utilisation of EBP, finite resources are not wasted on the delivery of ineffective interventions. Additionally, EBP limits the amount of disability and suffering throughout the community by ensuring the most current and effective care is provided.
1.5 What are the alternatives to evidence-based practice?
You may be wondering how nurses made decisions about their practice before the relatively recent EBP movement, or even what the alternatives to EBP are. If we are honest, for most of our working life we function on automatic pilot; that is, we ritualistically do things the way we have always done them, the way we were taught as a student or graduate nurse, or just in the accepted way of doing things in our current workplace.
However, at times our comfort zone is challenged, and we identify a knowledge deficit when confronting an unusual or challenging problem. At times like these, practitioners may guide their practice by asking the opinion of colleagues or senior practitioners, reviewing employer policies, reading textbooks or lecture notes, leafing through nursing or other journals, and listening to speakers at professional conferences or other education forums. Can you think of some benefits and limitations to these methods of guiding practice? For example, if a decision needs to be made immediately, guidance from an experienced colleague or organisational manual provides a quick and easy reference tool. However, on the downside, even well-meaning and senior practitioners may not have the latest knowledge, and policy manuals are frequently out-of-date, even if they were prepared using the best evidence at the time of policy development.
1.6 Why the rapid spread of evidence-based practice?
for the spread of the EBP movement have been the:
lack of research-based information to support clinical decision making
lack of research-based guidelines and protocols to use in clinical practice
overwhelming volume and variability of new journal information, and
inadequacy of traditional sources of information (e.g. textbooks out-of-date).
However, health departments around the world are increasingly being stretched to cover ever-rising health expenditures and, with treatment and care costs increasing all the time, governments need to ensure they are using public funds for treatment and care that is effective with positive health outcomes and benefits for the public.
).
While EBP was initially limited to the practice of medicine it became clear that unless all the members of the health team embraced EBP it would have limited impact.
1.7 Where is the evidence located?
Evidence for practice decisions is increasingly available in online format. Some resources are available free of charge, while others attract a fee for use, although staff and students of healthcare facilities and universities can usually access these through the institution at no personal cost. Many electronic resources now provide links to full-text journal articles for some records. New products are constantly being developed to allow practitioners to quickly and easily search for relevant evidence. Some of the currently well-established and recommended sources of evidence are described below.