Contents
Guide
Pagebreaks of the print version
The author and publisher have provided this e-book to you for your personal use only. You may not make this e-book publicly available in any way. Copyright infringement is against the law. If you believe the copy of this e-book you are reading infringes on the authors copyright, please notify the publisher at: us.macmillanusa.com/piracy.
Dedicated to
Randy
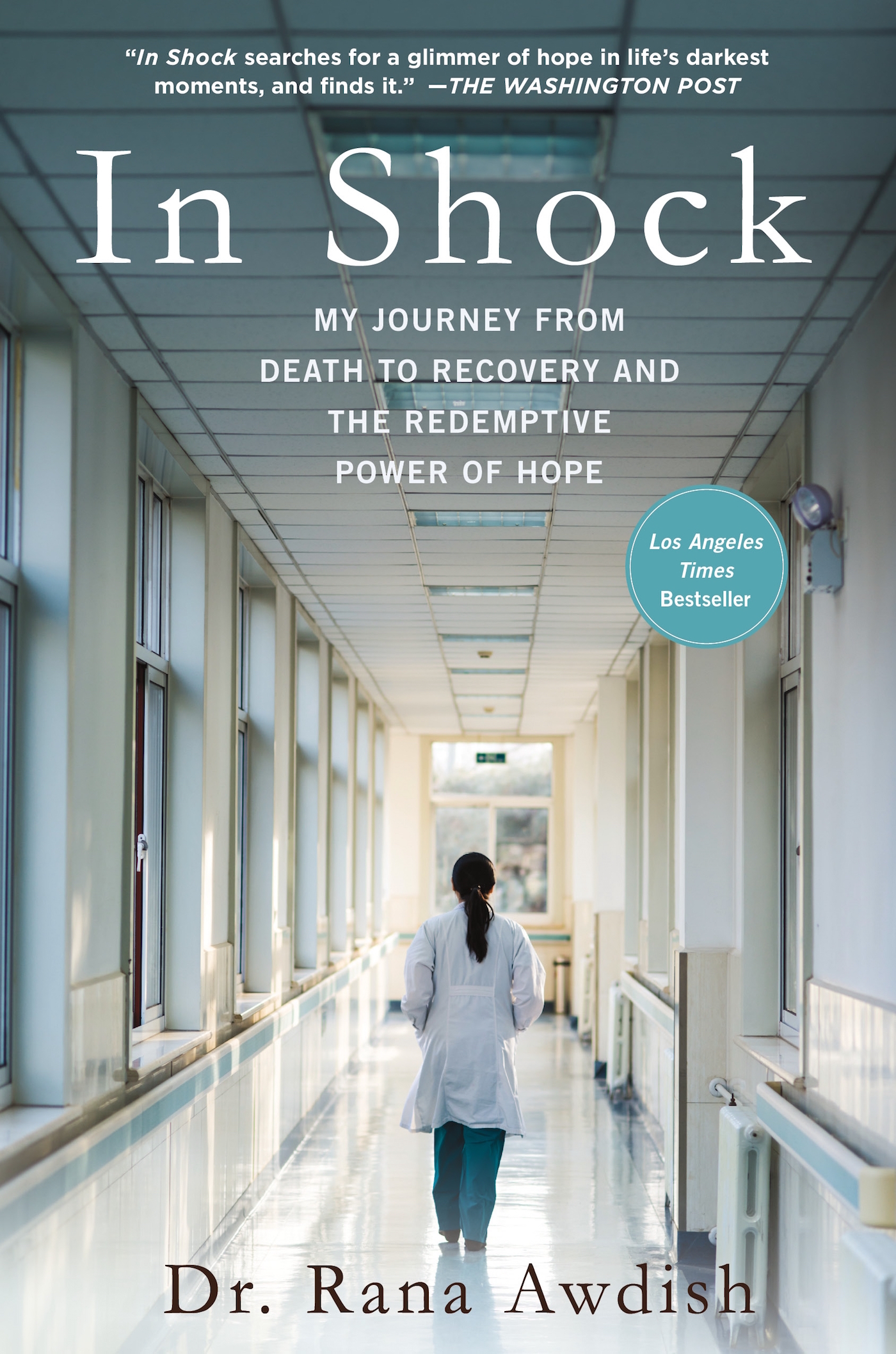
Medicine can be a magical lens through which to view the human body. Focus its light on an unsorted pile of symptoms and it will converge them neatly into a diagnosis. A swollen, red strawberry tongue in a feverish child will lead the doctor to examine the heart and affirm a diagnosis of vasculitis. A mans burning stomach pain transforms into gastritis, which has both a cause and a cure, whereas his nonspecific pain had neither.
Medicine does this by asking questions and listening for not just what is said, but what may be true. If empathy is the ability to take the perspective of another and feel with them, then, at its best, the practice of medicine is a focused, scientific form of empathy. Truly caring for a patient necessitates traversing borders and inhabiting the view of another with the humility of a visitor who knows he or she can choose to look away. They each possess the power to heal.
The first time I viewed the world through medicines transformative lens I was five years old, listening as my mother offered a seemingly vague description to the pediatrician by phone. My brother was leaning forward in the crib, onto his hands, drooling, and seemed to be gulping the air rather than breathing. The doctor understood this to be epiglottitis, an often fatal swelling of the airway. He instructed her with a calm but firm urgency to bring him immediately to the emergency room, where he would be waiting. That ability to translate symptoms into diagnoses and treatments, the power to save lives through knowledge and listening, struck me as the most beautiful job description I could imagine.
Attending medical school was like entering a secret society, complete with its own language, uniforms, and societal norms. We learned to translate the genetic code and sequence genes that produced proteins that made up organs. We were granted cadavers to dissect and study, each structures name rooted in ancient Latin or Greek. We spent a year immersed in the divine elegance of the human body, so that in our second year we could learn to recognize pathology. We were instructed by professors who spoke of the innate intelligence of disease. Parasites that exploited their host, small changes in genes that resulted in defective hearts, and endlessly replicating cancer cells. By learning the pathway to disease, we were taught, we could unlock cures. The knowledge was intoxicating. I followed the vectored curriculum, believing I would emerge transformed and able to heal.
I couldnt have imagined the circuitous form my training would actually take. The forward progression through residency and fellowship was nothing more than a comfortable lie my body would ultimately dismantle. My body somehow understanding that despite completing my training, despite being surrounded by every form and severity of disease, I had yet to learn what it meant to be sick. I would experience an illnessfollowed by a long, painful recoverythat took me apart, piece by piece, and put me back together in a conformation so different I questioned if I still existed at all.
The wish for the cure is seductive; it captivates and charms. Devastating illness, despite its ability to utterly transform, is not revered in the same way. Illness is viewed as an aberrant state. It is a town we drive through on a journey home, but not a place to stop and linger. We pass through with gritted teeth, as if it were a storm, with no regard for the illuminating beauty of the lightning as it strikes. But those shattering moments that break our bodies also allow us access to wisdom that is normally hidden, except in times of utter darkness.
From my new vantage point in an ICU bed, I would begin to sense a dark hole at the center of a flurry of what was otherwise highly proficient, astoundingly skillful care. I couldnt name it at first. I would have glimpses of clarity, only to have it recede out of focus. I had to train myself to see it, like negative space on a canvas. It took years of being a patient to understand that though the healing potential of knowledge is magical, it is also a lie.
Medicine cannot heal in a vacuum; it requires connection.
As a patient, its upending to be confronted with the actual fragility of everything you once believed to be a constant. To inhabit that vulnerable space, and to have no one around you who is open to discussion of the devastation is patently surreal. We all desire to be seen, to be known, to share our experiences and feel heard. To have our life events given context and meaning, redirected back to us in a way that we can understand and integrate into our understanding of who we believe ourselves to be. This need is more acute in times of sickness. When organs and limbs function without fail, we can indulge notions of self-reliance and agency. We believe ourselves to be the narrators of our own lives. When we are sick, we are humbled by our dependency on others, the loss of control, the uncertainty of the ending. This change opens channels for communication we are hardwired not to tune into during the monotonous routines and spaces of normal life.
Recognizing those open channels and fostering connection in full view of the knowledge is what heals. Making the choice to be present for someone elses suffering requires a kind of anticipatory resolve. Because it does get hard, sometimes even unbearably so. The choice to be present means deciding at the outset that you will be there for the duration. That premeditated sort of intentionality may not resonate with the kind of effortless empathy wed imagined, until we remind ourselves that all forms of love require work and a fierce commitment.
Had our training somehow taught us to avoid these channels? Did we know what to do when we recognized them?
I work at a large urban hospital, in the center of a busy and diverse city. We are sent patients, by helicopter and ambulance, who have run out of options elsewhere. The kind of clinical excellence, determination, and teamwork necessary to care for these uniquely complex patients far surpasses what Ive experienced in other hospitals during medical school or residency training. I have the great privilege of working at an amazing institution. The shared purpose and the pride that comes from doing hard work well is one of the reasons I chose to stay on after my fellowship training.
The hard times, the times when I knew we missed the mark, can almost always be understood and rationalized. Health care is exceedingly complex. Errors will inevitably occur, at even the best hospitals. What seems different to me is our transparent willingness to acknowledge that we are a learning organization. This orientation causes us to look honestly at each lapse, whether it be in communication or drug delivery. Acknowledge it, determine the point the process broke down, and address it. Perhaps it is because of our awareness that all systems attempting remarkable things will at times fail that weve learned to cultivate resilience. We never allow a failure, however small, to be the end of the story. Its always the beginning of a better way of being.