Springer International Publishing AG 2018
Jennifer T. Huang and Carrie C. Coughlin (eds.) Skin Tumors and Reactions to Cancer Therapy in Children
1. Melanoma and Spitz Nevi in Children
Melanocytic nevi are common skin neoplasms and can be either congenital or acquired. While congenital nevi can be present at birth or appear shortly thereafter, acquired nevi continue to develop through childhood and into early adulthood. In a large cross-sectional study of kindergarten children in Germany, nevi were noted to increase in number from a median of 3 at 2 years of age to 19 at 7 years of age []. Since these two groups have similar skin types, this highlights the role of sun exposure in the development of nevi.
In addition to the development of new nevi, existing nevi naturally evolve throughout childhood, and a change in appearance may be not be concerning for melanoma []. Although pediatric melanoma is uncommon, identifying clinically suspicious lesions is essential for timely diagnosis and treatment. Appropriately identifying concerning lesions is especially important in the pediatric population where biopsies may be relatively more emotionally or psychologically stressful. Spitz nevi and atypical Spitz nevi pose a particular challenge clinically and histologically because of features that overlap with melanoma. Research has focused on histologic, immunohistochemical, and genomic methods to differentiate between these three entities.
Spitz Nevi
Key Points
Most commonly found in the pediatric population.
Present as smooth pink, red, brown, or black papules that initially grow rapidly and then stabilize.
Composed of epithelioid and/or spindle cells.
In 1948, Dr. Sophie Spitz described a subset of pediatric melanocytic tumors that had features of melanoma but lacked their aggressive clinical characteristics []. Although previously called benign juvenile melanoma , this tumor is now called spindle and epithelioid cell nevus or, more commonly, Spitz nevus. A variant of the Spitz nevus is the pigmented spindle cell nevus (pigmented cell tumor of Reed, Reed nevus, pigmented Spitz nevus).
Clinical
Spitz nevi most commonly arise in patients less than 20 years of age [].
Fig. 1.1
Characteristic appearance of a Spitz nevus as a smooth dome-shaped pink papule []. Reprinted from Journal of the American Academy of Dermatology, Vol. 65, No. 6, Luo S, Sepehr A, Tsao H, Spitz nevi and other Spitzoid lesions: Part I. Background and Diagnoses, pages 10731084, 2011, with permission from Elsevier
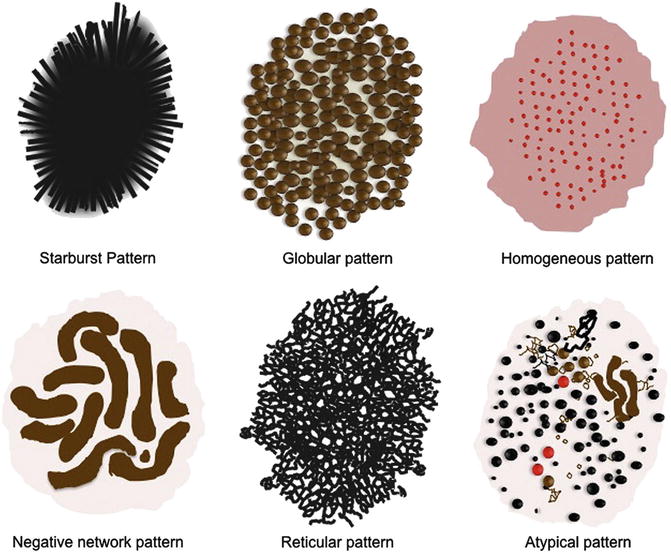
On dermoscopy, Spitz nevi have several common patterns, including starburst, globular, homogeneous, negative network, and reticular patterns (Fig. ]. Common melanoma-specific structures, such as atypical pigment network, negative network, crystalline structures, blue-white veil, and irregular vessels, have been described in Spitz nevi but are more likely to be symmetric and organized.
Fig. 1.2
Common dermoscopy patterns seen in Spitz nevi []. Reprinted from Dermatologic Clinics, Vol. 31, No. 2, Kerner M, Jaimes N, Scope A, Marghoob AA, Spitz nevi: a bridge between dermoscopic morphology and histopathology, pages 327335, 2013, with permission from Elsevier
Histology
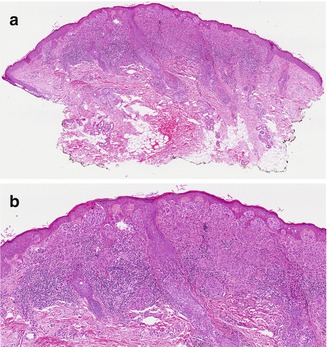
While the majority of Spitz nevi are compound, they can also be junctional or intradermal. At low power, Spitz nevi are dome or wedge shaped, symmetric, and well-circumscribed. At higher power, Spitz nevi have characteristic epithelioid and/or spindled melanocytes with prominent cytoplasm. Junctional cells are nested and often have clefts separating individual cells or nests from adjacent epidermis. Cells mature to become small individual melanocytes deeper in the dermis. Kamino bodies are acellular pale eosinophilic structures often found within the epidermis and are composed of basement membrane material. Epidermal hyperplasia, hyperkeratosis, and hypergranulosis are commonly seen. Occasional mitotic figures can be seen within the epidermis or superficial dermis, although deep mitoses can indicate a more atypical tumor ( Fig. ) . Pigmented spindle cell nevi resemble Spitz nevi histologically but have prominent cytoplasmic pigmentation.
Fig. 1.3
Spitz nevus. ( a ) At low power, the characteristic wedge-shaped, symmetric, well-circumscribed architecture of a Spitz nevus is seen (H&E, 40). ( b ) Junctional and dermal nests of mostly epithelioid and some spindled melanocytes are seen. Eosinophilic globules ( Kamino bodies) are in the epidermis, and there is mild epidermal hyperplasia. Lymphohistiocytic inflammation is present in the dermis (H&E, 100) (Image courtesy of Adam I. Rubin, MD)
Genetics
Approximately 20% of Spitz nevi demonstrate an increase in chromosome 11p, which is the site of the HRAS gene []. Gain of this genetic locus is very rare in cutaneous melanoma. Gain of chromosome 11p therefore suggests a more benign etiology (see Genetics and Molecular Analysis below). Apart from an occasional gain in HRAS , genetic gains or losses are rare in Spitz nevi.
Management
Although generally considered to be benign, controversy exists surrounding the management of Spitz nevi. For classic appearing Spitz nevi in school-aged children, some advocate for clinical observation, while others advocate a biopsy of any Spitzoid lesion []. Though, if re-excision is pursued, narrow 12 mm margins are adequate.
Atypical Spitz Tumors
Key Points
Histologic features overlapping with Spitz nevi and melanoma.
Molecular testing with fluorescence in situ hybridization and/or comparative genomic hybridization is an adjunct to histologic evaluation.
HRAS mutations, BAP1 mutations , and kinase fusions have been identified in these tumors.
Atypical Spitz tumors (AST), also called Spitzoid tumors of uncertain malignant potential (STUMP) , are challenging because they have histologic features that overlap with both classic Spitz nevi and with melanoma. Consequently, the diagnosis and management of these tumors are controversial and still evolving.
Atypical Spitz tumors are often considered within the larger category of borderline melanocytic tumors or melanocytic tumors of unknown malignant potential (MelTUMP). The term MelTUMP was first used by Elder and Xu to encompass a wide spectrum of lesions that demonstrate features of both benign melanocytic nevi and melanoma []. In addition to AST, pigmented epithelioid melanocytoma, deep penetrating nevus, and cellular blue nevus are the most common neoplasms included in this group.