Springer International Publishing Switzerland 2016
Porcia B. Love and Roopal V. Kundu (eds.) Clinical Cases in Skin of Color Clinical Cases in Dermatology 10.1007/978-3-319-23615-5_1
1. Discoid Lupus Erythematosus
Case Presentation
A 30-year old African American woman presents with multiple scarred plaques on her scalp, ears, and neck. The lesions are occasionally pruritic and even painful, especially in the early stages when they first appear. She notes that outbreaks are worse during the summer, and she admits that she is very conscious of her appearance year-wide, often wearing her hair past her shoulders and clothing that covers her neck to help hide her skin. She denies joint pain, shortness of breath, chest pain, or ever noticing any ulcers in her mouth.
Physical Examination
On examination, polymorphic, round to oval shaped hyper- and hypopigmented patches are found scattered on her face and neck, some with adherent scale (Fig. ).
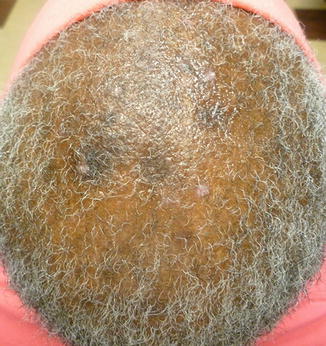
Figure 1.1
( a , b ) Discoid lupus of the scalp and face. Polymorphic, round to oval shaped hyper- and hypopigmented patches are found scattered on her face and neck, some with adherent scale. She also has indurated, atrophic, scarred, depigmented plaques on the eyebrows, cheeks, and conchal bowls of the ears ( a ). A scarred, indurated plaque is noted on the occipital scalp ( b )
Differential Diagnosis
During its earlier stages, discoid lesions may not have developed characteristic features such as follicular plugging, and they may present as erythematous and inflamed indurated plaques. At this point, they can be confused with psoriasis, although psoriasis presents with well demarcated erythematous plaques with silvery scale and well-defined edges on the scalp, elbows and knees. The plaques of lichen planus are more violaceous with characteristic Wickhams striae. Polymorphous light eruption presents with tiny erythematous papules or plaques on sun exposed areas and burning or pruritus; however, the face is usually spared. Granuloma annulare presents with erythematous indurated annular plaques with a raised border, typically on the dorsal surface of the fingers, hands, feet, or elbows. Both early and late stages of discoid lesions may also be confused with sarcoidosis (Walling and Sontheimer ). However, sarcoidosis is characterized by erythematous or violaceous, indurated plaques and nodules that usually affect the nose, cheeks, ears, and lips. Sarcoidosis may be accompanied by pulmonary abnormalities.
Pathology
Punch biopsy of an active lesion on the ear revealed the following characteristics: (1) epidermal atrophy, (2) hyperkeratosis, (3) mononuclear inflammatory cell infiltrate (mostly lymphocytes) at the subepidermal junction, and (4) thickening of the basement membrane containing mucin vacuoles. Scalp biopsy revealed (1) follicular plugging with keratin, (2) reduced number of follicle units, (3) dermal perivascular and perifollicular lymphocytic infiltrate, (4) interstitial fibrosis, and (5) basal membrane degeneration with keratinocyte necrosis (Elder ).
Direct immunofluorescence of a lesional site is positive for immunoglobulin (mainly IgM) and complement deposition at the dermoepidermal junction (Elder ).
Laboatory Studies
Blood serological testing was negative for ANA, anti-Ro, anti-Sm, and dsDNA.
Diagnosis
Discoid lupus erythematosus (subtype of chronic cutaneous lupus erythematous)
Case Treatment
A thorough discussion of the diagnosis, natural history, and treatment options for discoid lupus were discussed with the patient. The patient was started on a high dose prednisone taper for 1 month. After having an ophthalmology exam, she was started on hydroxychloroquine 200 mg twice daily. Side effects, including retinopathy and liver function abnormalities were discussed. Clobetasol 0.05 % ointment was recommended on the discoid lesions twice a day. She was given strict instructions regarding daily sun protection, including a wide brimmed hat, sunglasses, sun protective clothing, and a broad spectrum sunscreen with an SPF of 30. She was also advised to avoid excess sun exposure between the hours of 10 am and 2 pm. Smoking should also be avoided as patients with lupus who smoke do not respond well to treatment.
Discussion
Discoid lupus erythematosus (DLE) is the most common form of cutaneous lupus erythematous (CLE), accounting for the largest subtype of chronic CLE (1). It is slightly more common in African Americans, Hispanics, and Asians than Caucasians (Petri ).
Figure 1.2
( a , b ) Discoid lupus of the body. Hyperpigmented plaques with scarring, atrophy, and depigmentation are noted on the arm ( a ) and back ( b ) with atrophy. As these lesions spread over time, plugging from the adherent keratin scale can be seen as well as dyspigmentation (hyperpigmented borders, hypopigmentation at center) ( a ). Older, healed lesions present with dermal atrophy and telangiectasia in the center, leaving behind a depressed scar ( b )
Figure 1.3
Discoid lupus of the scalp. Hyperpigmented plaques with adherent scale and dyspigmentation are noted on the scalp
Cutaneous lupus erythematous (CLE) encompasses a broad spectrum of lupus-specific skin pathology characterized by inflammation primarily mediated by infiltrating T lymphocytes incited by an unclear mechanism comprising of a number of genetic, environmental, and hormonal factors (Hordinsky ).
CLE can be present with or without systemic lupus erythematous (SLE). Different forms of CLE carry different risks of systemic involvement. Discoid lupus carries the lowest risk compared to other forms of CLE (Hordinsky ).
It is important to note that in patients with skin of color who have systemic lupus erythematous (SLE), skin involvement may be the predominant clinical finding, particularly discoid lupus. The Hopkins Lupus cohort followed over 1500 SLE patients in Baltimore and found that African Americans with SLE were more likely to have cutaneous manifestations compared to Caucasians. DLE was significantly more common in African Americans, whereas photosensitivity, malar rash, and mouth ulcers were less common compared to their Caucasian counterparts (Petri ). If clinical suspicion for SLE is high based on history and exam findings, screening for serological markers (ANA, anti-Ro, anti-Sm, and dsRNA) or referral for more extensive work-up is indicated.