Contents
VIII. DRUGS FOR ENDOCRINE DISORDERS
56 Drugs for Diabetes Mellitus
MARSHAL SHLAFER
DIABETES MELLITUS: OVERVIEW OF THE DISEASE AND ITS TREATMENT
The term diabetes mellitus is derived from the Greek word for fountain and the Latin word for honey. Hence, the term describes one of the prominent symptoms of untreated diabetes: production of large volumes of glucose-rich urine. Indeed, very long ago, the disease we now call diabetes was diagnosed by the sweet smell of urineand, yes, by its sweet taste as well. In this chapter we use the terms diabetes mellitus and diabetes interchangeably.
Diabetes is primarily a disorder of carbohydrate metabolism. Symptoms result from a deficiency of insulin or from cellular resistance to insulin's actions. The principal sign of diabetes is sustained hyperglycemia, which results from impaired glucose uptake by cells and from increased glucose production. When hyperglycemia develops, it can quickly lead to polyuria, polydipsia, ketonuria, and weight loss. Over time, hyperglycemia can lead to hypertension, heart disease, renal failure, blindness, neuropathy, amputations, impotence, and stroke. In addition to affecting carbohydrate metabolism, insulin deficiency disrupts metabolism of proteins and lipids as well.
Diabetes is a major public health concern. In the United States, diabetes is the most common endocrine disorder, and the sixth leading cause of death by disease. According to the Centers for Disease Control and Prevention, 23.6 million Americans have diabetes, and nearly one-quarter of them have not been diagnosed. Another 57 million Americans are prediabetic, and hence are at increased risk of developing diabetes in the future. In 2007, diabetes cost the U.S. economy an estimated $174 billion ($116 billion in direct medical expenditures and $58 billion in lost productivity). These costs represent a 32% increase over the estimated costs for 2002. Put another way, the total cost of diabetes is going up by roughly $8.4 billion every year.
Types of Diabetes Mellitus
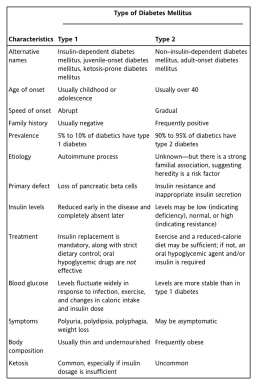
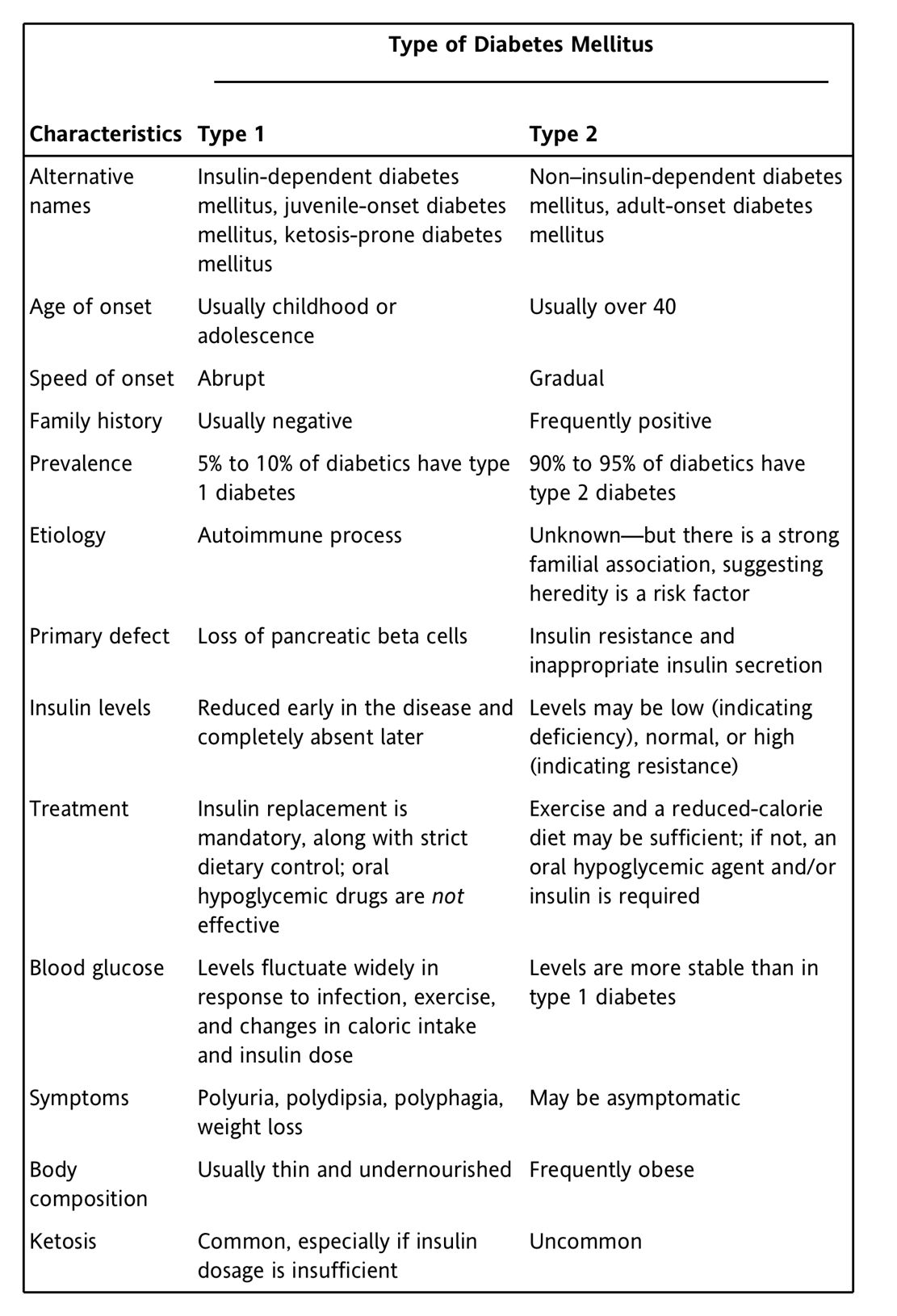
There are two main forms of diabetes mellitus: type 1 diabetes mellitus and type 2 diabetes mellitus. Both forms have similar signs and symptoms. Major differences concern etiology, prevalence, treatments, and outcomes (illness severity and deaths). The distinguishing characteristics of type 1 and type 2 diabetes are summarized in Table 56-1 and discussed immediately below. Another important formgestational diabetesis discussed below under Diabetes and Pregnancy.
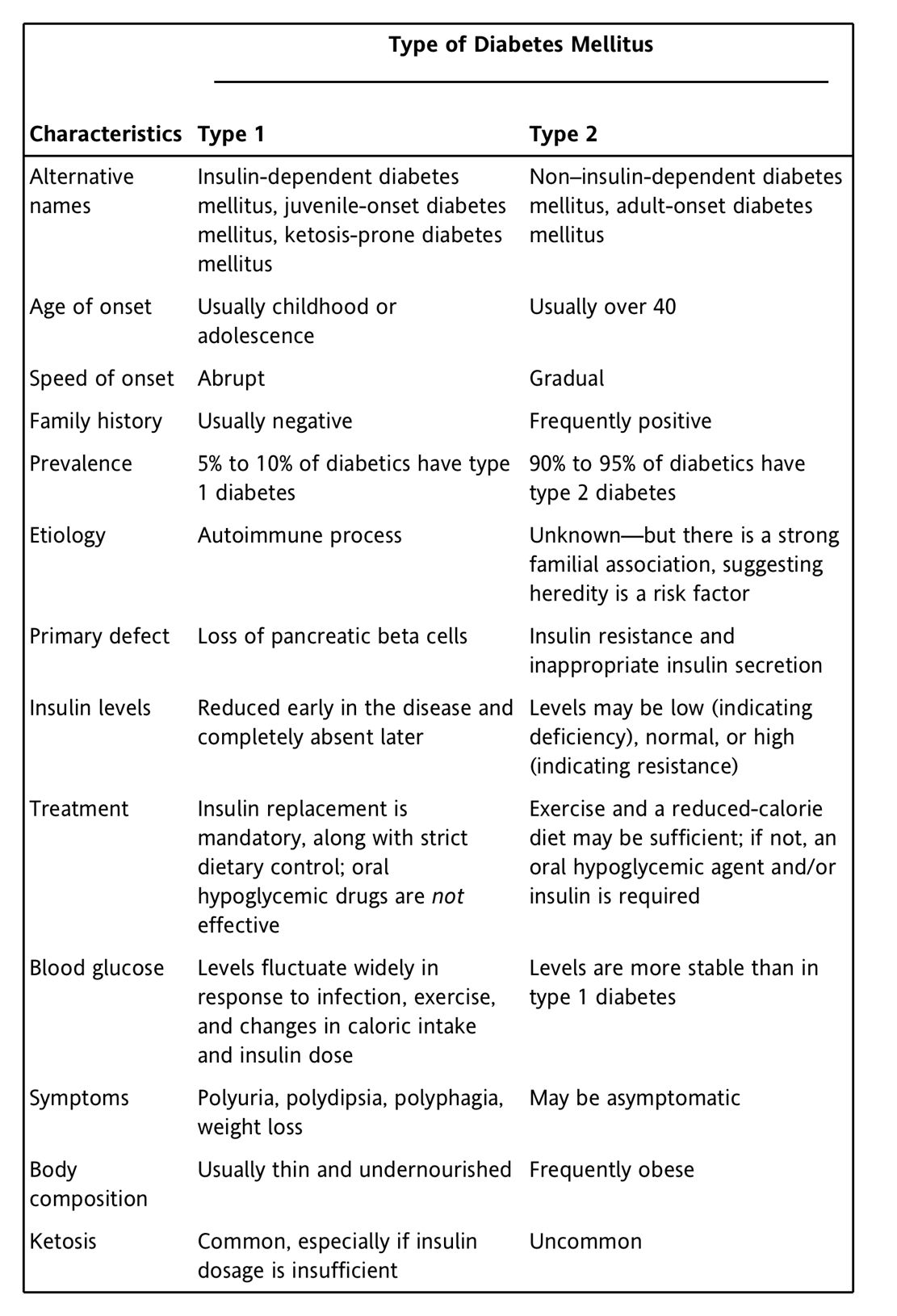
TABLE 56-1 Characteristics of Type 1 and Type 2 Diabetes Mellitus
Type 1 Diabetes
Type 1 diabetes accounts for about 5% to 10% of all diabetes cases. Between 1.2 million and 2.4 million Americans have this disorder. In the past, type 1 diabetes was called insulin-dependent diabetes mellitus (IDDM) or juvenile-onset diabetes mellitus. As a rule, type 1 diabetes develops during childhood or adolescence. Onset of symptoms is relatively abrupt.
The primary defect in type 1 diabetes is destruction of pancreatic beta cellsthe cells responsible for insulin synthesis. Insulin levels are reduced early in the disease and fall to zero later. Beta cell destruction is the result of an autoimmune process (ie, development of antibodies against the patient's own beta cells). The trigger for this immune response is unknown.
Type 2 Diabetes
Type 2 diabetes is the most prevalent form of diabetes. Approximately 22 million Americans have this disease. In the past, type 2 diabetes was called noninsulin-dependent diabetes mellitus (NIDDM) or adult-onset diabetes mellitus. The disease usually begins in middle age and progresses gradually. Obesity is almost always present. In contrast to type 1 diabetes, type 2 diabetes carries little risk of ketoacidosis. However, type 2 diabetes does carry the same long-term risks as type 1 diabetes (see below).
Symptoms result from a combination of insulin resistance and impaired insulin secretion. In contrast to patients with type 1 diabetes, those with type 2 diabetes are capable of insulin synthesis. In fact, insulin levels tend to be normal or slightly elevated. However, although insulin is still produced, its secretion is no longer tightly coupled to plasma glucose content: release of insulin is delayed and peak output is subnormal. More importantly, the target tissues of insulin (liver, muscle, adipose tissue) exhibit insulin resistance. Resistance appears to result from three causes: reduced binding of insulin to its receptors, reduced receptor number, and reduced receptor responsiveness. Over time, hyperglycemia leads to destruction of pancreatic beta cells, and hence insulin production and secretion eventually decline.
Although the underlying cause of type 2 diabetes is unknown, there is a strong familial association, suggesting that genetics may be a major factor. This possibility was reinforced by a study that implicated the gene for insulin receptor substrate-2 (IRS-2), a compound that helps mediate intracellular responses to insulin. Mice that lack a functional IRS-2 gene develop symptoms identical to those of type 2 diabetes (eg, insulin resistance in muscle and liver, fasting hypoglycemia, and gradual beta cell failure).
Short-Term Complications of Diabetes
Acute complications are seen mainly in type 1 diabetes. Principal concerns are hyperglycemia and hypoglycemia. Hyperglycemia results when insulin dosage is insufficient. Conversely, hypoglycemia results when the insulin dosage is excessive. Ketoacidosis, a potentially fatal acute complication, develops when hyperglycemia is allowed to persist. As noted above, ketoacidosis is rare with type 2 diabetes, and relatively common in patients with type 1 diabetes. All three complications are discussed below.
Long-Term Complications of Diabetes
The long-term sequelae of type 1 and type 2 diabetes take years to develop. More than 90% of diabetic deaths result from long-term complications, not from hypoglycemia or ketoacidosis. Ironically, among patients with type 1 diabetes, insulin therapy can be viewed as having made long-term complications possible: Prior to the discovery of insulin, these people died long before chronic complications could arise.
Most long-term complications occur secondary to disruption of blood flow, owing to either macrovascular or microvascular damage. There is strong evidence that tight control of blood glucose can reduce microvascular injury. Tight glycemic control also reduces macrovascular injury, although other measures (eg, exercise, healthy diet, control of blood pressure and blood lipids) are also important.
Macrovascular Damage
Cardiovascular disease (CVD) is the leading cause of death among diabetic patients. Diabetes carries an increased risk of heart disease, hypertension, and stroke. Much of this pathology is due to atherosclerosis, which develops earlier in diabetics than in nondiabetics and progresses at a faster rate. Macrovascular complications result from a combination of hyperglycemia and altered lipid metabolism.
Microvascular Damage
Damage to small blood vessels and capillaries is common. The basement membrane of capillaries thickens, causing blood flow in the microvasculature to fall. Destruction of small blood vessels contributes to kidney damage, blindness, and various neuropathies. Microvascular injury is directly related to the degree and duration of hyperglycemia.
Retinopathy.
Diabetes is the major cause of blindness among American adults. Every year, 12,000 to 24,000 diabetics lose their sight. Visual losses result most commonly from damage to retinal capillaries. Microaneurysms may occur, followed by scarring and proliferation of new vessels; the overgrowth of new retinal capillaries reduces visual acuity. Capillary damage may also impair vision by causing local ischemia, which can kill retinal cells. Retinopathy is accelerated by hyperglycemia, hypertension, and smoking. Accordingly, these risk factors should be controlled or eliminated. All patients with diabetes, whether type 1 diabetes or type 2 diabetes, should have a comprehensive eye exam (preferably by an ophthalmologist) at least once a year.
Next page