Contents
Part 1: Neurological Critical Care
Stuart McGrane, MBChB, MSCI, Pratik P. Pandharipande, MD, MSCI, and Christopher G. Hughes, MD
Fred Rincon, MD, MSc, MBE, FACP, FCCP, FCCM
Scott A. Marshall, MD, and Geoffrey S. F. Ling, MD, PhD, FAAN
Sherry H-Y. Chou, MD, MMSc, FNCS
Part 2: Cardiovascular Critical Care
Antoinette Spevetz, MD, FCCM, FACP, and Joseph E. Parrillo, MD, FACC, MCCM
Michael R. Pinsky, MD, CM, Dr h.c., FCCP, MCCM
Felix Y. Lui, MD, and Kimberly A. Davis, MD, MBA
Chapter 8: Severe Heart Failure, Cardiogenic Shock, and Pericardial Tamponade
(Including Principles of Intra-aortic Balloon Pumps and Ventricular Assist Devices)
Etienne Gayat, MD, PhD, and Alexandre Mebazaa, MD, PhD
Sachin Yende, MD, MS, David T. Huang, MD, MPH, and R. Phillip Dellinger, MD, MCCM
Deepa M. Patel, MD, and Craig M. Coopersmith, MD
Fredric Ginsberg, MD, FACC, FCCP, and Joseph E. Parrillo, MD, FACC, MCCM
Ravi Agarwala, MD, FRCPC, Sean Patrick Whalen, MD, and Natalie Bradford, MD
Chapter 13: Valvular Heart Disease, Acute Aortic Dissection, and Patient Care
After Cardiac Surgery
Michael H. Wall, MD, FCCM, and Pamela R. Roberts, MD, FCCM
Amanda M. Gomes, MD
Marcos Emanuel Gomes, MD, and Pamela R. Roberts, MD, FCCM, FCCP
Stylianos Voulgarelis, MD, and Sylvia Y. Dolinski, MD, FCCP
Part 3: Respiratory Critical Care
Nicholas C. Watson, MD, and Stephen O. Heard, MD
Eric Ursprung, MD, and Theofilos P. Matheos, MD
Debasree Banerjee, MD, MS, Jeffrey Mazer, MD, and Nicholas Ward, MD
Jennifer A. LaRosa, MD, FCCM, FCCP, and R. Phillip Dellinger, MD, MCCM
Neil R. MacIntyre, MD
Kenneth E. Wood, DO, and Jason A. Stamm, MD
Scott E. Kopec, MD, FCCP, and Marie T. Mullen, MD
Robert A. Balk, MD
Part 4: Critical Care Infectious Diseases
Ryo Yamamoto, MD, and Ramon F. Cestero, MD, FACS
Gourang Patel, PharmD, MSc, and Anand Kumar, MD
Gloria Vazquez-Grande, MD, and Anand Kumar, MD
Shravan Kethireddy, MD, Anna Chen, MD, Jonathan Perez, MD, and Mary Jane Reed, MD, FCCM
Part 5: Hepatic, Gastrointestinal, Hematologic/Oncologic Disease in the ICU
Vinod P. Balachandran, MD, and Soumitra R. Eachempati, MD, FACS, FCCM
Adil M. Abuzeid, MBBS, and Nabil M. Issa, MD
Mario Raul Villalba, MD, FACS, and Martin A. Schreiber, MD, FACS
John Crommett, MD, and Joseph L. Nates, MD, MBA, FCCM
Part 6: Renal and Metabolic Disorders in the ICU
Chapter 33: Acute and Chronic Renal Failure and Management (Including Hemodialysis and
Continuous Renal Replacement Therapies)
Michael L. Bentley, PharmD, FCCM, FCCP, FNAP, and Ashita J. Tolwani, MD, MSc
Alisha Bhatia, MD, and David M. Rothenberg, MD, FCCM
Linda L. Maerz, MD, FACS, FCCM
Gozde Demiralp, MD, and Pamela R. Roberts, MD, FCCM, FCCP
Nestor Arita, MD, Jeremy L. Ward, MD, and Paul E. Marik, MD, FCCM, FCCP
Pamela R. Roberts, MD, FCCM, FCCP
Part 7: Environmental and Toxicologic Injury
Todd Huzar, MD, and James M. Cross, MD, FACS
Michael Sirimaturos, PharmD, BCNSP, BCCCP, FCCM, Rebeca L. Halfon, BS, PharmD, and
Janice L. Zimmerman, MD, MCCM, FCCP
Janice L. Zimmerman, MD, MCCM, FCCP
Part 8: Pharmacologic Issues in the ICU
Quinn A. Czosnowski, PharmD, and Craig B. Whitman, PharmD, BCPS, BCCCP
Brian L. Erstad, PharmD, MCCM, and Courtney McKinney, PharmD
Part 9: Surgical and Obstetrical Critical Care
Yatin Mehta, MD, Jaya Sugunaraj, MD, Mark A. Kleman, DO, M. Camilla Bermudez, MD, Heather J. Johnson, PharmD, Patricio Andres Sanchez-Cueva, MD, and Mary Jane Reed, MD, FCCM
Sherry Sixta, MD, and Rosemary Kozar, MD, PhD
Christina C. Kao, MD, Tashinga Musonza, MD, Lillian S. Kao, MD, MS, and S. Rob Todd, MD
Jennifer E. Hofer, MD, Karen C. Patterson, MD, and Michael F. OConnor, MD, FCCM
Part 10: Administrative and Ethical Issues in the Critically Ill
Sara R. Gregg, MHA, and Timothy G. Buchman, MD, PhD, MCCM
Jean-Louis Vincent, MD, PhD, FCCM
Andrew M. Naidech, MD, MSPH
Fred Rincon, MD, MSc, MBE, FACP, FCCP, FCCM
CHAPTER 1
Altered Mental Status During Critical Illness: Delirium and Coma
Stuart McGrane, MBChB, MSCI, Pratik P. Pandharipande, MD, MSCI, and Christopher G. Hughes, MD
Key words: delirium, coma, Confusion Assessment Method for the Intensive Care Unit (CAM-ICU), Intensive Care Delirium Screening Checklist (ICDSC), Richmond Agitation-Sedation Scale (RASS)
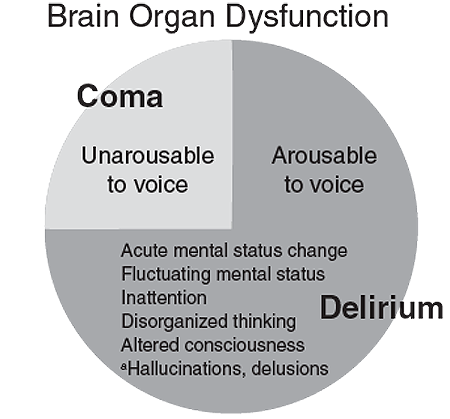
Critically ill patients often manifest varying degrees of altered mental status secondary to their acute disease processes or as a consequence of the therapies used to treat disease. These mental status changes range from coma to hyperactive delirium. A comatose patient is unresponsive to physical or verbal stimuli, whereas delirium is an acute and fluctuating disorder of consciousness characterized by inattention, disorganized thinking, and perceptual disturbances ( Figure 1 ). Alterations in mental status have traditionally been considered expected consequences of critical illness, and clinicians are increasingly aware that these mental status changes are manifestations of acute brain organ dysfunction that are associated with worse clinical outcomes. Early studies evaluating coma and delirium were hampered by the many different terms (eg, confusional state, ICU psychosis, acute brain dysfunction , and encephalopathy ) used to describe altered mental status during critical illness. Additionally, the lack of validated bedside tools (besides the comprehensive Diagnostic and Statistical Manual of Mental Disorders ) to diagnose delirium prevented the incorporation of delirium monitoring into routine clinical care in the ICU.
Figure 1. Delineation between delirium and coma, highlighting the cardinal symptoms of delirium
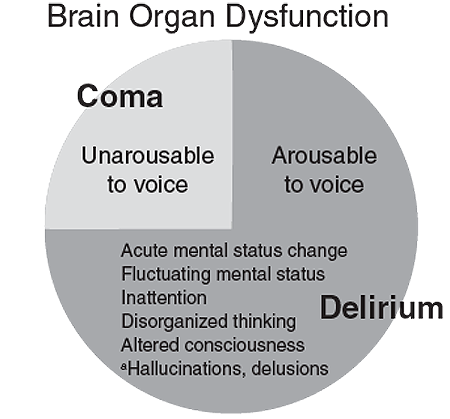
aOptional symptoms of delirium (may be present but are not required for the diagnosis of delirium).
DIAGNOSIS OF ACUTE BRAIN DYSFUNCTION
Traditionally, many scales have been available to assess the level of sedation and agitation in ICU patients, including the Ramsay scale, Riker Sedation-Agitation Scale (SAS), motor activity assessment scale, and Richmond Agitation-Sedation Scale (RASS). The recent guidelines on pain, agitation, and delirium from the Society of Critical Care Medicine recommend the use of the RASS and SAS due to their psychometric properties and validity in critically ill patients. The RASS ( Figure 2 ) also has been shown to detect variations in the patients level of consciousness over time or in response to changes in sedative and analgesic drug use. As a first step in assessing the level of consciousness, a sedation-agitation scale should be used. Patients who are unresponsive to verbal commands (eg, a RASS -4 or-5) are considered to be in a coma and cannot be evaluated for delirium at that time. Patients who are responsive to verbal stimuli (eg, RASS -3 and lighter) can further be evaluated for the content of that arousal via the use of delirium monitoring instruments.
Figure 2. The Richmond Agitation-Sedation Scale (RASS)
Score | Term | Description |
+4 | Combative | Overtly combative, violent, immediate danger to staff |
+3 | Very agitated | Pulls or removes tubes or catheters; aggressive |
+2 | Agitated | Frequent nonpurposeful movement, fights ventilator |
+1 | Restless | Anxious but movements not aggressive or vigorous |