1.1 Introduction
Brain tumors are divided into primary (70%) and secondary (30%). About 24,000 primary brain tumors are diagnosed each year in the United States and account for 20% of malignancies before 15 years. The estimated incidence is 8.2 per 100,000 people. Although these tumors are not common (<1.5% of all cancers) in comparison with tumors of other organs (e.g., lung, breast, or colon), they deserve a unique position in tumor oncology because of their histopathologic complexity and biologic behavior. Noteworthy is the fact that despite their low incidence they have a high mortality among adult cancer patients and even more in children [].
Topographical and histological classifications, as well as correlations of topography to pathology, serve for the better studying, understanding, and handling of brain tumors. They are found in any location and in patients of any age. Differences in epidemiology, location, and pathology between children and adults make it necessary to take into consideration the age parameter, and to consider adult and pediatric brain tumors separately.
As a result for any therapeutic decision or prognostic determination, all these factors, that is, age, location, and pathology have to be combined.
1.2 Epidemiology
1.2.1 Pediatric Brain Tumors
Fifteen to 20% of all intracranial tumors occur in children under 15 years of age, with the peak occurrence between 4 and 8 years of age. The incidence of brain tumors in children has been estimated to be 2.5 per 100,000 people per year, the vast majority of them being primary. Only 12% of all brain tumors occur in children under 2 years of age [].
In neonates, brain tumors are uncommon, represent congenital tumors, and have a different histologic and topographic distribution compared with those that occur in young children and adolescents. They are more likely to be developed in the supratentorial region than in the posterior fossa. The most common primary brain tumors in the neonatal period are teratomas, embryonal tumors, and congenital glioblastoma multiforme [].
In children between the ages of 2 and 10 years, primary brain tumors are generally more benign than those found in neonates. Seventy percent of these tumors are developed beneath the tentorium [].
About 30% of posterior fossa tumors in children are cerebellar astrocytomas (most often pilocytic), 3540% are medulloblastomas (arising for more than 90% in the vermis of the cerebellum), 25% are brain stem gliomas, and 1015% are ependymomas of the fourth ventricle.
In children younger than 3 years of age, 30% of all intracranial tumors are ependymomas []
1.2.2 Adult Brain Tumors
The incidence of primary brain tumors appears to have increased, particularly in the elderly people of developed countries, during the last 25 years. The incidence of primary malignant brain tumors increased by 40% in the general population and 100% in the elderly (more than 65 years of age) in the United States and Canada [].
Gliomas in man and meningiomas in woman are the most common primary brain tumors constituting respectively 60 and 20% of all intracranial tumors in adults. In adults, tumors of glial origin are the most frequent primary neoplasms [].
Approximately 8085% of all intracranial tumors in adults occur in the supratentorial region. The primary tumors are 5075% of all tumors, while metastases account for the remainder. The infratentorial tumors in adults are mainly extra-axial lesions [].
Approximately 50% of the intracranial tumors are gliomas. Most of them (70%) are astrocytic tumors, and more than 50% of these are anaplastic or glioblastoma multiforme [].
The primary posterior fossa tumors in adults are either intra- or extra-axial. The three most common tumors are schwannoma, meningioma, and epidermoid tumor. All of these tumors are extra-axial. The most often intra-axial primary brain tumor in adults is hemangioblastoma and brain stem glioma. The metastatic intra-axial tumor in the posterior fossa is the most common tumor in this region. In this location, metastatic tumors account for 1520% of all intracranial metastases [].
1.3 Clinical Course
Brain tumors produce symptoms and signs due to direct tissue destruction, local brain infiltration, or secondary effects of increased intracranial pressure. The symptoms of patients are dependent on the anatomic location of the tumor. Negative symptoms include loss of function, and positive symptoms seizures or headache.
Headache is the first symptom in 35% of patients and with growing of the tumor it is present in up to 70% of patients. Usually, it is associated with vomiting or nausea, papilledema due to increased intracranial pressure or focal cerebral signs.
Facial pain may be present with tumors at the base of the skull or nasopharynx.
Seizures are the first symptom in 30% of brain tumors and account for 5% of all patients with epilepsy. Seizure frequency is seen in up to 95% of patients with oligodendrogliomas and occurs in only 18% of patients with metastatic brain tumors [].
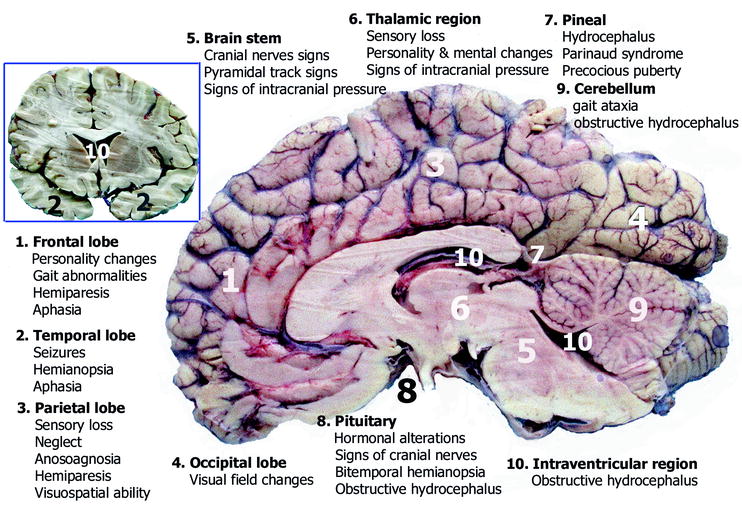
Focal clinical signs: The clinical manifestations of brain tumors depend on the location of tumor in the brain (Fig. ).
Fig. 1.1
Coronal ( upper left ) and sagittal ( right ) autopsy specimens of the brain show the clinical signs of the brain tumors in relation to their location
Fig. 1.2
Sagittal autopsy specimen of the brain shows the distribution most of the primary intracranial tumors in childhood and adulthood
Frontal lobe tumors cause personality changes, gait abnormalities, hemiparesis, and aphasia.
Temporal lobe tumors more often cause seizures. Temporal hemianopsia and aphasia may be present.
Parietal lobe tumors cause sensory loss, neglect, anosoagnosia, hemiparesis, and disturbances of visuospatial abilities.
Occipital lobe tumors cause visual field changes.
Brain stem tumors commonly present with cranial nerve and pyramidal track signs, as well as symptoms and signs associated with increased intracranial pressure.
Thalamic tumors present with sensory loss, personality and mental changes, as well as symptoms and signs of increased intracranial pressure.
Pineal tumors produce symptoms and signs of hydrocephalus, Parinaud syndrome, and precocious puberty.
Pituitary tumors may present with hormonal alterations, symptoms and signs of cranial nerves, bitemporal hemianopsia, and obstructive hydrocephalus.