Bruce R. Smoller and Kim M. Hiatt Inflammatory Dermatoses: The Basics 10.1007/978-1-4419-6004-7_1 Springer Science+Business Media, LLC 2010
1. Superficial Perivascular Dermatitis
Bruce R. Smoller 1
(1)
Department of Pathology, University of Arkansas for Medical Sciences, 4301 W. Markham Street, Little Rock Arkansas, 72205, USA
Bruce R. Smoller (Corresponding author)
Email:
Abstract
Superficial perivascular dermatitis
Inflammatory dermatoses involving venules in superficial vascular plexus
Other histologic changes help with further classification
Superficial perivascular dermatitis (SPD)
Without epidermal changes
Superficial perivascular dermatitis
Superficial perivascular dermatitis (SPD)
Without epidermal changes
Lymphocytic infiltrate
Mixed infiltrate
Pigmented purpuric eruption, Schamberg variant (progressive pigmentary dermatosis)
Clinical
Erythematous, non-blanching patches
Usually on lower extremities, pre-tibial
Most common in middle-aged men
May be related to drug exposure in some cases
Controversial relationship with mycosis fungoides
Multiple subtypes of pigmented purpuric eruption
Histologic findings
Superficial perivascular lymphohistiocytic infiltrate
Eosinophils not common
Mild spongiosis and exocytosis
Hemorrhage and hemosiderin surrounding vessels in superficial vascular plexus
Perls iron or Prussian blue stain often helpful in demonstrating dermal hemosiderin deposition (necessary to document chronicity of process) (Figs. )
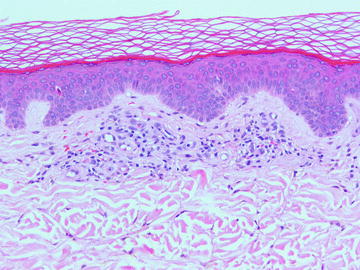
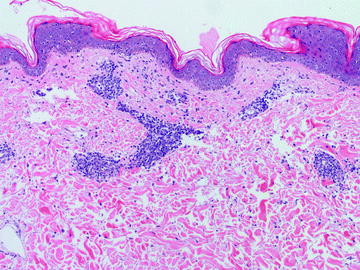
Fig. 1.1
Pigmented purpuric eruption, Schamberg variant, shows a mild superficial perivascular lymphohistiocytic infiltrate. Erythrocyte extravasation is present. The overlying epidermis is uninvolved
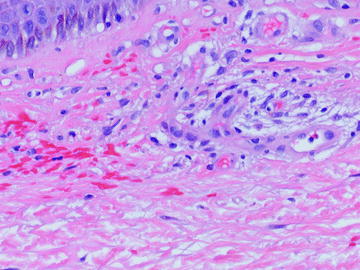
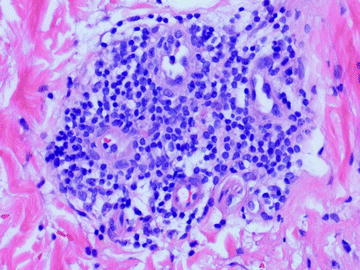
Fig. 1.2
Pigmented purpuric eruption, Schamberg variant. This high-power image shows perivascular erythrocyte extravasation. Hemosiderosis is variable, depending on the duration of disease, and can be nearly non-existent as in this case
Viral exanthem
Clinical
Morbilliform (measles-like) eruption
Erythematous papules and macules usually rapid onset
Resolves rapidly without sequelae in most cases
Histologic findings
Superficial perivascular lymphohistiocytic infiltrate
Inflammation does not usually extend into deeper dermis
Eosinophils very uncommon
Slight exocytosis, epidermal spongiosis, and basal vacuolopathy
Occasional dying keratinocytes, but very few
Non-specific findings hard to establish diagnosis without clinical correlation (Figs. )
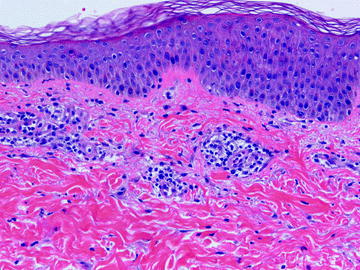
Fig. 1.3
This viral exanthem shows a superficial perivascular lymphohistiocytic infiltrate with no alterations in the overlying epidermis
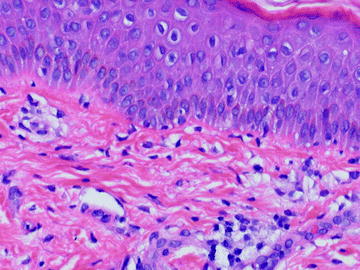
Fig. 1.4
Mild spongiosis and interface degeneration are seen in this viral exanthem
Gyrate erythema
Clinical
Most commonly refers to erythema annulare centrifugum, but also includes erythema gyratum repens, erythema chronicum migrans, other less common eruptions
Annular, erythematous lesions on trunk
Slow outward extension of plaques in some cases
Peripheral, delicate scale
Histologic findings
Almost entirely lymphoid infiltrate in a perivascular distribution
Eosinophils may rarely present in small numbers
Tight cuffing of lymphocytes around vessels of the superficial vascular plexus
Some cases also involve deeper vascular plexus
Scant parakeratotic scale with mild underlying spongiosis if peripheral scale is biopsied
Plasma cells present in small numbers in erythema chronicum migrans, but not usually in erythema annulare centrifugum (Figs. )
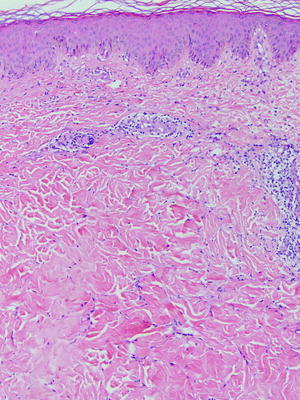
Fig. 1.5
Erythema annulare centrifugum is characterized by a lymphohistiocytic infiltrate tightly cuffed around the vessels
Fig. 1.6
Erythema annulare centrifugum characteristically has a lymphohistiocytic infiltrate. Plasma cells may be seen; neutrophils and eosinophils are not characteristic
Fig. 1.7
Erythema chronicum migrans shows a superficial perivascular lymphohistiocytic infiltrate without significant epidermal involvement