Deborah F. MacFarlane (ed.) Skin Cancer Management A Practical Approach 10.1007/978-0-387-88495-0_1 Springer Science+Business Media, LLC 2009
1. Biopsy Techniques and Interpretation
Deborah F. MacFarlane 1 and Ronald P. Rapini 2
(1)
Departments of Dermatology and Plastic Surgery, The University of Texas MD Anderson Cancer Center, Houston, TX, USA
(2)
Department of Dermatology, University of Texas Medical School, Houston, TX, USA
Abstract
The performance of a skin biopsy is an intrinsic part of the initial management of a patient suspected of having a skin cancer.1,2 This first chapter will therefore begin with a discussion of the various skin biopsy techniques most commonly used in the diagnosis of skin cancer and their clinical indications. This will be followed by a frank discussion of the interpretation of biopsy results. Discussion of other biopsy techniques such as curettage and sentinel lymph node biopsy will be dealt with elsewhere (Chapters 6 and 15, respectively).
The performance of a skin biopsy is an intrinsic part of the initial management of a patient suspected of having a skin cancer., respectively).
Biopsy Technique
Pre-Op
Before performing a biopsy, it is important to have taken a medical history and performed a physical exam. The presence of potential problems such as coagulopathies, drug allergies including lidocaine allergies, artificial joints, and heart valves should be ascertained (). Most biopsy procedures can be safely performed in patients on warfarin, heparin, clopidogrel bisulfate, aspirin, and non-steroidal anti-inflammatory drugs if sufficient care is taken and hemostatic agents are available. The risks and benefits of the biopsy should be explained and consent obtained.
Site Preparation and Anesthesia
The site should next be cleansed with an antiseptic such as isopropyl alcohol, povidone-iodine, or chlorhexidine, for example. Local anesthesia is best performed with a 30-gauge needle used to slowly infiltrate a buffered lidocaine solution. Most physicians utilize 1% lidocaine with 1:100,000 epinephrine. A buffered lidocaine solution can be less painful, and for larger procedures the 0.5% lidocaine solution reduces the possibility of toxicity that may occur when large amounts of lidocaine are used. One common dilution is 9 parts of 0.5% lidocaine with 1:200,000 epinephrine to one part of the standard available sodium bicarbonate solution. With such a dilute concentration of epinephrine, one does not need to worry about potential interactions between epinephrine and beta-blockers for instance, and patients do not experience the tachycardia that sometimes occurs with a stronger epinephrine solution.
Hemostasis
For biopsy sites that are not sutured, styptic agents are often used. Ferric subsulfate (Monsels solution) may pigment the tissue, complicating histologic interpretation and aluminum chloride hexahydrate (Drysol) is preferable. The styptic is applied on a cotton-tipped swab with pressure to the biopsy site and held in place for several seconds and reapplied if necessary. Another alternative in a freely bleeding biopsy site is to apply a piece of hemostatic sponge, such as Gelfoam, and to bandage the site.).
Shave Biopsy
In this technique the superficial layer of the skin is sampled and it is therefore minimally invasive and usually not associated with significant scarring. It can be used in the diagnosis of superficial skin cancers such as actinic keratoses (AK), squamous cell carcinoma in situ (SCCIS), and basal and squamous cell carcinomas (BCC and SCC). One disadvantage of this technique is that tumor existing deep to the plane of the shave can be missed (see Table
Table 1.1
Biopsy techniques
Biopsy type | Lesion |
|---|
Shave | AK, BCC, SCC |
Saucerization | Pigmented lesions, SCC |
Punch | SCCIS to check for invasion |
Incisional | Melanoma in situ to check for invasion |
Wedge | Ulcerated SCC |
Excisional | Atypical nevi, melanoma |
Reproduced from Rapini (1994) with permission from Elsevier.
Equipment
A number 15 blade, toothed forceps, hemostatic agent, cotton-tipped applicator, gauze, and bandage. Please note that a razor blade may also be substituted for a number 15 blade.
Technique
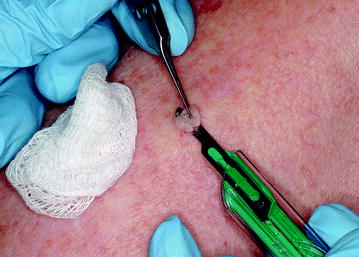
After cleansing the area, the local anesthetic is slowly infiltrated to raise a wheal. The skin is stabilized using the first and second fingers of the non-dominant hand, then the belly of the blade is held against the skin in a horizontal position and a gentle sawing motion is used to slowly separate the specimen and some surrounding skin from its base (Fig.
Hemostasis is achieved; the biopsy site is then dressed with an application of antibiotic ointment or petrolatum and covered with a dressing, which is changed daily for approximately 1 week until the area has healed.
Complications
Hypopigmentation and cutaneous depression may occur if the biopsy is deep.
Saucerization
In a saucerization biopsy, a razor blade is bent into a U-shape to obtain a deeper specimen. This is indicated for the biopsy of lesions reaching the upper to mid-dermis such as SCC, atypical nevi, and superficial melanoma.
Equipment
A Gillette super blue razor blade and the same equipment as used with the shave biopsy.
Technique
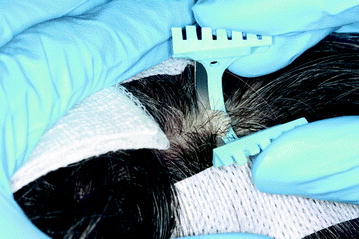
After cleansing and infiltrating the area as previously described, the razor blade is bent into a U-shape and held between the first two fingers of the dominant hand. A sawing motion is used to obtain the biopsy (Fig. ). Hemostasis and aftercare are as previously described.
Fig. 1.2
Saucerization biopsy. Note hair is taped down to facilitate biopsy
Punch Biopsy
Punch biopsy is useful for providing information about the depth of tumor invasion as, depending on the size of punch used, it can reach subcutaneous tissue. A 3-mm punch is standard, but 6- and 8-mm punches may be used for removing larger lesions. A 2-mm punch is most often used for cosmetically sensitive areas such as the face, but may be harder to process in the lab and may give an inadequate sample for diagnostic purposes, especially for melanocytic neoplasms.
Equipment
Sterile punch, scissors, toothed forceps, suture.
Technique
Prepare and anesthetize the skin as previously described. Next, stabilize the skin by stretching it taut between the first and second fingers of the non-dominant hand and perpendicular to the relaxed skin tension lines, creating an oval defect, which can be more easily sutured. Holding the punch between the first two fingers of the dominant hand, place the punch on the area to be biopsied so that all edges of the punch are in contact with the skin. Rotate the punch between the fingers pressing down at the same time until there is a loss of resistance and the subcutaneous plane is reached (Fig.